All published articles of this journal are available on ScienceDirect.
Efficacy of Supramolecular Salicylic Acid 30% Combined with Intense Pulsed Light Compare to Monotherapy Supramolecular Salicylic Acid 30% in Acne Vulgaris Patients
Abstract
Background:
Acne is one of the most common inflammatory skin diseases. Treatment of acne has been challenging due to the multiple factors involved in its pathogenesis. To date, there are several treatments available. They are traditional chemical peeling, laser-based therapy, and so on. Therefore, as several studies reached inconsistent conclusions on which treatment was better, this observational study aimed to compare the efficacy of monotherapy supramolecular salicylic acid (SSA) and the combination of SSA with intense pulsed light (IPL) treatment in acne patients.
Methods:
43 patients with acne vulgaris were chosen at the outpatient department of dermatology from October 2019 until December 2020. Patients were divided into 2 groups: group 1, with a total of 23 patients who underwent SSA 30% combined with IPL, and group 2, which will do monotherapy with SSA 30%. Chemical peeling with SSA 30% treatment will be done every 2 weeks, while IPL treatment will be performed every 4 weeks for a treatment course of 8 weeks. Each individual had a VISIA skin examination and an investigator global assessment (IGA) of acne severity scores every four weeks to evaluate clinical improvement and treatment efficacy.
Results:
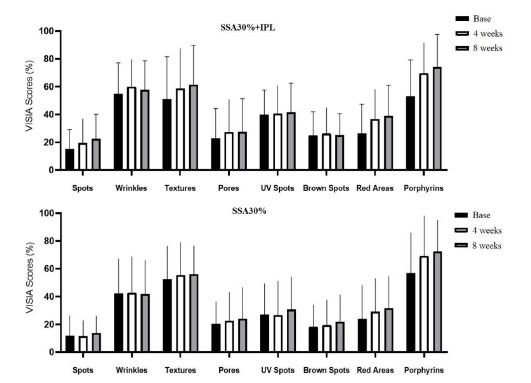
Patients in the SSA 30% + IPL group were mostly female, with comparable baseline VISIA skin scores. During 8-week intervals, the SSA 30%+IPL group presented with a greater improvement in overall skin condition measured by VISIA compared to the SSA 30% alone. Although both groups have a positive effect on skin condition improvement, when it comes to acne, gradual improvement in porphyrins and red areas was more obvious in the combined SSA 30%+IPL group compared to SSA 30% alone.
Conclusion:
The combination of SSA 30% with IPL compared to SSA 30% alone not only provides better treatment for acne vulgaris but also improves skin rejuvenation.
1. INTRODUCTION
Acne is one of the most frequent inflammatory skin diseases encountered by dermatologists. Four factors are involved in the development of acne: follicular hyperkeratinization, resulting in a keratin plug and leading to the formation of comedones; an increase in sebum production; and Cutibacterium acnes bacteria, which digests lipids in sebum and attracts various cytokines, leading to an inflammatory papule and inflammation [1, 2]. Acne, in general, has been classified into several subtypes. The first form of acne is comedones, which consist of blackheads and whiteheads [3]. The second form of acne is inflammatory. These are the red spots, such as papules, nodules, pustules, and cysts [1, 3]. The third is hormonal acne; a woman predominantly gets it, along with the beard distribution in men, like the jawline, cheek, and even neck area. Lastly, nodulocystic acne leads to sinus infections, abscesses, and extensive scarring. Acne may be classified as mild, moderate, or severe depending on the type, amount, and size of the lesions [4]. Although the most severe acne is not a life-threatening condition, we have to consider the impact of acne on lowering self-esteem, triggering psychological distress, and ultimately decreasing health-related quality of life [5].
A recent study indicates that the prevalence of acne in mainland China in 2016 was around 39.2%, with an upward trend in adolescence due to puberty [6]. However, puberty was not the only factor; other factors such as genetic, environmental, and psychological conditions may also play a role in acne development, thus creating the treatment of acne affected by many variables and uncertain [7]. In other countries, such as the United States of America, the first line of acne treatment is usually benzoyl peroxide, a topical retinoid, or a combination of topical medications consisting of benzoyl peroxide and an antibiotic (erythromycin or clindamycin), a retinoid, or both [8]. However, the main method that hospitals in China typically use when dealing with acne vulgaris is different. For instance, the use of intense pulse light (IPL) and salicylic acid is preferred compared to conventional treatment. Therefore, this study aims to compare the treatment efficacy of supramolecular salicylic acid (SSA) 30% alone with IPL combined with SSA 30% in Asian patients with acne vulgaris.
2. METHODS
43 patients (37 women and 6 men) with Fitzpatrick skin types III–IV presenting with acne vulgaris were randomly selected from October 2019 to December 2020, with an age range of 18–48 years. Patients were divided into 2 groups: the first group consisted of 23 patients receiving SSA 30% and intense pulsed light treatment (IPL), while the second group (n = 20) receiving monotherapy with SSA 30%. Patients under other acne treatments (oral therapy, light therapy, or laser therapy) were excluded from this study. Chemical peeling with SSA 30% treatment would be done every 2 weeks, while IPL treatment will be performed every 4 weeks for a treatment course of 8 weeks. A VISIA skin analysis and an investigator global assessment (IGA) of acne severity scores were performed every 4 weeks on each subject to evaluate clinical improvement and efficacy of the treatment. The study was performed in accordance with the principles of the Declaration of Helsinki, and the research protocol was approved by the institutional ethical review board of the first affiliated hospital of Chongqing Medical University (April 29, 2020, No. 2020-233).
Before the treatment, all patients cleansed their facial skin using a mild cleansing cream. After that, data imaging was performed by VISIA skin analysis in the first affiliated hospital of Chongqing Medical University's Laser Department. IPL treatment (Lumenis M22 System, Lumenis Ltd.) with expert filters at 590nm wavelength, triple pulse mode (4.0 ms), and energy range between 10 and 13 J/cm2 was followed by comedone extraction with an acne needle, chemical peeling with SSA 30%, and blue light therapy (BLT) for 15 minutes in group 1. Group 2 treatment, on the other hand, included comedone extraction with an acne needle, chemical peeling with SSA at 30%, and BLT treatment with a 470 nm (10 nm) blue LED for 15 minutes. Following treatment, all patients were advised to use a medical-grade facial mask for 30 minutes and to apply Sun Protector Factor (SPF) daily. During the 4 and 8 weeks of treatment, each participant was scheduled for a follow-up. During the follow-up, participants were advised to first cleanse their facial skin by using a mild cleansing cream, and then VISIA skin analysis and IGA acne severity score examinations were performed every 4 weeks (Fig. 1).
Method of application, supramolecular salicylic acid 30%: Based on the manufacturer’s instructions, an appropriate amount of SSA (7 g/box) was added to a small therapeutic bowl. The main component of the therapeutic agent was SA combined with Poloxamer 407 as an emulsifiable paste via supramolecular technology (Broda, Shanghai Rui Zhi Medicine Technology Co., Ltd.; patent numbers US8865143 and EP2689774), with an initial concentration of 5-8%. After adding normal temperature water (25o C) (2ml), SSA was released from Poloxamer 407 and reached a concentration of 30%. After stirring, the chemical substance was applied to the skin lesions. Sites to avoid for SSA application include the eyes, nasal cavities, and lips. After 10-20 minutes, the chemical substance was rinsed with water.
Data collection: For clinical imaging and skin analysis, VISIA® (CANFIELD Imaging Systems, Fairfield, NJ, USA) is required to analyze skin conditions such as skin texture, spots, brown spots, ultraviolet (UV) spots, porphyrins, red areas, pores, and wrinkles through size and definition. The images are taken from the front view and at 45o to the left and right lateral views before and after the treatment. An investigator global assessment (IGA) was performed to categorize acne severity and evaluate the acne condition. According to investigator global assessment scores for acne severity, acne severity has been categorized into four grades: grade I (clear), grade II (mild severity), grade III (moderate severity), and grade IV (severe).
Endpoint: The main outcome in this study was a comparison of patients’ acne improvement (including spots, textures, pores, red areas, and porphyrins) between SSA 30% combined with IPL and SSA 30% alone. The secondary outcome was an improvement in the patient’s wrinkles, UV spots, and brown spots with SSA 30% combined with IPL versus SSA 30%.
Statistical analysis: Data were analyzed by using SPSS version 25.0 (IBM, USA). Data were expressed as median and interquartile boundary values or means ± standard deviation (SD) as appropriate. Comparison between pre-and post-treatment of SSA 30% against SSA 30% combined with IPL was made by using GraphPad PRISM 8.4.
3. RESULTS
From October 2019 to December 2020, a total of 43 consecutive patients were diagnosed with acne vulgaris. In addition, the patients were divided into two groups based on the treatment they received. The first group was SSA 30% combined with IPL (n = 23), and the second group was SSA 30% alone (n = 20). After the first treatment, a VISIA skin score will be done every four weeks to monitor the skin's progress.
Table 1 shows the baseline characteristics of this study, where the patients were divided into 2 groups. The SSA 30%+IPL group participants were predominantly female compared to the SSA 30% alone (95.6% vs. 75.0%). Baseline VISIA and IGA acne severity scores between IPL combined with SSA 30% and SSA 30% alone were comparable, with similar IGA acne severity scores between the 2 groups, while on VISIA skin scores, only wrinkles and UV spots were presented with a significant gap between the 2 groups (54.88% ± 22.22 vs. 42.27% ± 26.00, 39.84% ± 17.85 vs. 27.05% ± 23.08, respectively).
In terms of the main and secondary outcomes of this study, the SSA 30%+IPL group showed a higher improvement in every indicator measured by VISIA compared to the SSA 30% alone. In Fig. (2), improvement of spots (22.49% ± 17.67 vs. 13.88% ± 13.32), wrinkles (57.88% ± 20.77 vs. 41.78% ± 25.18), textures (61.46% ± 28.20 vs. 56.27% ± 21.54), pores (27.55% ± 23.90 vs. 24.12% ± 23.05), UV spots (41.57% ± 21.14 vs. 30.73% ± 24.67), brown spots (25.30% ± 15.21 vs. 21.98% ± 20.23), red areas (39.09% ± 21.95 vs. 31.73% ± 24.22), and porphyrins (74.30% ± 23.26 vs. 72.47% ± 23.47) were more prominent in the SSA 30%+IPL group.
Figs. (3 and 4) show the patient's pre- and post-treatment skin condition, with spots and texture improvement in the IPL+SSA 30% group being more prominent compared to the SSA 30% group. Meanwhile, Figs. (S1-S4) show images of the patient's red areas and porphyrins before and after treatment. All of the pictures were taken by VISIA skin analysis, and skin improvement was better in the SSA 30%+IPL group.
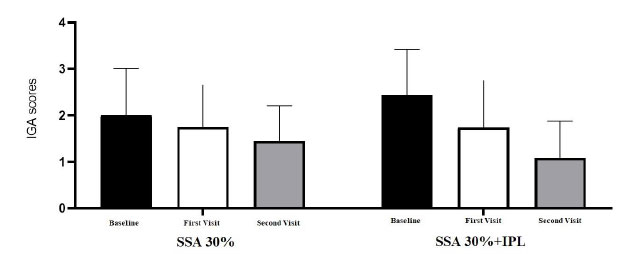
The comparison of the IGA acne severity scores of the two groups is shown in Fig. (5). Baseline IGA acne scores were comparable between SSA 30% alone and SSA 30%+IPL (2.00±1.01 vs. 2.43±0.99, respectively). There were no significant differences in IGA acne severity scores between the two groups at the first post-treatment visit. However, in the second visit, there were significant changes in the IGA acne severity scores, favoring SSA 30% combined with IPL (1.45±0.76 vs. 1.09±0.79, respectively).
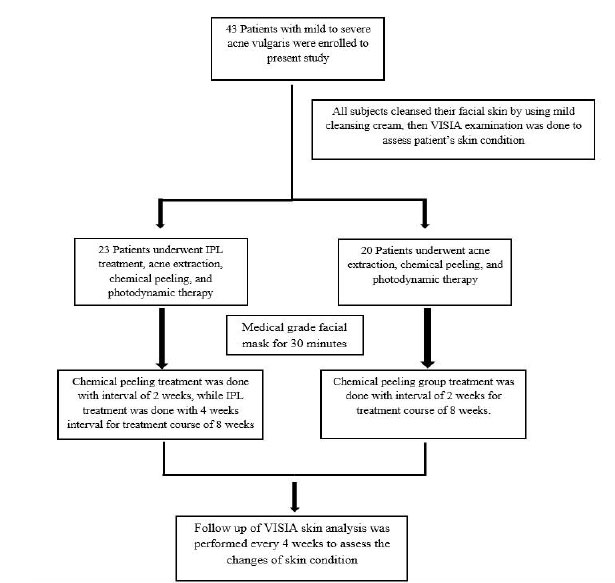
Table 1.
| Baseline Characteristics | SSA 30%+IPL (n=23) | SSA 30% (n=20) |
|---|---|---|
| Age | 27.78 ± 7.43 | 23.92 ± 5.51 |
| Female (%) | 95.6 | 75 |
| Skin Condition | - | - |
| Spots (%) | - | - |
| Left | 9.0 (1.0 – 13.0) | 2.5 (1.0 – 7.5) |
| Front | 16.0 (8.0 – 56.0) | 10.0 (2.3 – 29.3) |
| Right | 5.0 (1.0 – 12.0) | 1.5 (1.0 – 8.5) |
| Average | 15.33 ± 13.90 | 9.05 ± 19.28 |
| Wrinkles (%) | - | - |
| Left | 58.0 (23.0 – 74.0) | 24.5 (5.8 – 65.3) |
| Front | 51.0 (16.0 – 76.0) | 49.0 (16.5 – 68.8) |
| Right | 71.0 (42.0 – 85.0) | 43.0 (14.0 – 77.3) |
| Average | 54.88 ± 22.22 | 42.27 ± 26.00 |
| Texture (%) | - | - |
| Left | 52.0 (20.0 – 87.0) | 54.0 (30.5 – 78.0) |
| Front | 46.0 (23.0 – 85.0) | 59.5 (27.8 – 74.8) |
| Right | 59.0 (23.0 – 85.0) | 62.5 (30.3 – 76.3) |
| Average | 50.96 ± 30.66 | 52.57 ± 24.89 |
| Pores (%) | - | - |
| Left | 19.0 (5.0 – 44.0) | 21.5 (7.5 – 32.0) |
| Front | 10.0 (5.0 – 27.0) | 10.5 (5.3 – 19.0) |
| Right | 14.0 (4.0 – 40.0) | 14.5 (9.5 – 29.5) |
| Average | 22.80 ± 21.58 | 20.38 ± 17.02 |
| UV Spots (%) | - | - |
| Left | 36.0 (31.0 – 54.0) | 18.0 (8.3 – 33.8) |
| Front | 52.0 (24.0 – 62.0) | 23.5 (12.0 – 37.8) |
| Right | 36.0 (22.0 – 47.0) | 21.5 (10.5 – 34.0) |
| Average | 39.84 ± 17.85 | 27.05 ± 23.08 |
| Brown Spots (%) | - | - |
| Left | 17.0 (12.0 – 24.0) | 12.0 (5.3 – 25.0) |
| Front | 28.0 (11.0 – 48.0) | 14.5 (9.5 – 24.5) |
| Right | 19.0 (9.0 – 32.0) | 12.0 (7.0 – 22.8) |
| Average | 25.14 ± 16.80 | 18.33 ± 16.45 |
| Red Areas (%) | - | - |
| Left | 12.0 (5.0 – 38.0) | 11.5 (2.3 – 20.8) |
| Front | 37.0 (11.0 – 63.5) | 28.5 (7.3 – 56.0) |
| Right | 8.0 (5.0 – 29.0) | 10.0 (4.3 – 35.0) |
| Average | 26.29 ± 21.1 | 24.12 ± 24.91 |
| Porphyrins (%) | - | - |
| Left | 55.0 (38.0 – 83.0) | 60.5 (32.8 – 90.8) |
| Front | 31.0 (18.0 – 73.0) | 54.0 (14.3 – 87.3) |
| Right | 56.0 (34.0 – 82.0) | 59.5 (33.9 – 90.8) |
| Average | 53.13 ± 26.01 | 56.78 ± 30.36 |

4. DISCUSSION
The present study demonstrated that the combination of SSA 30% with IPL was not only safe but also more effective for acne vulgaris treatment and skin rejuvenation compared to SSA 30% alone. This finding is significant because it shows that a combination of treatments may speed up the healing of acne vulgaris and boost the patient's self-esteem.
Chemical peeling has become the cornerstone of treatment for acne vulgaris in this era. The main reason is due to its effect on inducing skin keratolysis and comedolytic effects. Not only that, chemical peeling may also decrease sebum production and pore size, along with anti-inflammatory and anti-bacterial properties [7, 8]. To date, several comedolytic agents are widely used for the treatment of acne vulgaris, for example, salicylic acid, benzoyl peroxide, Jessner’s solution, pyruvic acid, trichloroacetic acid (TCA), etc. However, it is still unknown which chemical peeling agent is best for acne treatment. Dayal et al. [9] found that 30% SA peels were more effective than Jessner’s solution in the treatment of comedones in acne vulgaris patients [53.4% vs. 26.3%, p = 0.001, respectively]. Abdel et al.’s [10] study found no significant difference between TCA and 30% SA for improvement of all lesions [RR 0.89; 95%CI 0.73, 1.10], while Jaffary et al.’s [11] study demonstrated similar efficacy for reducing comedones between 30% SA and 50% pyruvic acid [MD 7.45, 95%CI -18.46, 33.36]. To conclude, a recent meta-analysis performed by Chen et al. [12] found that commonly used chemical peels appear to be similarly effective and well-tolerated.

Typically, salicylic acid is used with ethanol as a chemical peeling agent. As a result, it might induce skin irritation and dryness and diminish the therapeutic efficacy of SA. Supramolecular salicylic acid (SSA) is a groundbreaking discovery in which weakly water-soluble salicylic acid is converted into water-soluble salicylic acid in the form of intermolecular complexes [13]. When applied to the skin, the water-soluble SA tends to be more bioavailable, decrease oil production, smooth skin surfaces, and produce less skin irritation [13, 14]. Several concentrations of SSA may be used as chemical peeling agents. However, the penetration depth and intensity of SSA peels improve with concentration, and several studies have confirmed that SSA (30%) is safe for superficial facial acne peeling [15]. Therefore, due to its better safety profile and treatment effect, SSA 30% was selected as the main chemical peeling agent for this study.
In the last two decades, the use of innovative laser or light-based treatments in the treatment of acne vulgaris has received significant attention. Several studies show that laser treatments with certain wavelengths have a photothermolysis effect, and when applied to the skin pores, the light energy is absorbed by porphyrin to generate reactive oxygen species (ROS). In addition, ROS will generate bactericidal effects by interfering with P. acnes' chemical and metabolic responses [16-18].
The two primary kinds of photodynamic treatment (PDT) are blue light and red light PDT. Owing to the fact that red light photodynamic treatment (PDT) penetrates deeper skin tissue and the majority of acne occurs in the superficial skin layer, blue light photodynamic therapy (PDT) is more appropriate due to its targeted area and safety profile. PDT alone has been identified as one of the alternate acne vulgaris therapies. Comparing the blue light phototherapy group to the 5% benzoyl peroxide group, Arruda et al. [19] found comparable effectiveness with fewer side effects in the blue light phototherapy group. Alba et al. [20] discovered that the number of comedones, pustules, and papules was decreased much more in the PDT group than in the 10% salicylic acid chemical peeling group.
Intense pulsed light (IPL) works the same way as photodynamic therapy for acne vulgaris treatment. Several studies have supported the use of IPL in acne patients. Chang et al. [21], for example, compared benzoyl peroxide gel to IPL for acne treatment and discovered no significant differences between the two groups. However, red macules, irregular pigmentation, and skin tone were improved in 63% of the laser-treated versus 33% of the benzoyl peroxide group. Yeung et al.'s [22] study showed the IPL group had a higher reduction of non-inflammatory lesions compared to the PDT group (38% vs. 43%, respectively). Unfortunately, a recent meta-analysis by Lu et al. [23] found that IPL efficiency is poorer than PDT treatment, and differences in geographic regions may affect IPL efficiency.
Although PDT and intense pulsed light (IPL) work the same way, a combination of PDT and IPL was possible based on the mechanism of IPL to cover the absorption peaks of porphyrins (400, 510, 542, 578, 630, and 665 nm) [24]. Rojanamatin et al. [25] found IPL-PDT to provide greater and longer-lasting acne improvement compared to IPL alone. Mei et al.'s [26] study demonstrated IPL plus PDT is more effective for moderate to severe acne vulgaris compared to IPL alone. Our finding was in agreement with previous findings, where the combination of IPL+PDT+SSA (30%) demonstrated higher improvement in acne and skin tone compared to PDT+SSA (30%).
The precise mechanism by which IPL, BLT, and SSA 30% interact with each other to improve acne vulgaris is still unknown. Moreover, research conducted in this area of study is still limited. Therefore, more large studies are needed to confirm our findings.
There are several unavoidable limitations to this study. First, our study consists of one treatment session and a short follow-up period. Second, this is a single-center observational study and therefore has its limitations in nature. Third, the additional aspects that may influence the success of the treatment cannot be ignored, for example, the work environment, skincare agents, cosmetics, foods, etc. Fourth, the present study was conducted with only a small number of samples and also lacked supporting evidence on the use of SSA 30% combined with IPL for acne vulgaris treatment. Therefore, large studies are still needed to confirm the significance of our finding.
CONCLUSION
The combination of SSA 30% with IPL compared to SSA 30% alone provides not only better treatment for acne vulgaris but also improves skin rejuvenation.
AUTHOR CONTRIBUTIONS
A.A and Y.M.C designed and performed the experiments, derived the models, and analyzed the data.
A.A, Y.H.P and J.C contributed to the design of the study.
A.A, Y.J.Z, L.Z.Z, X.Y.S and J.Y.C contributed for data extraction
A.A wrote the manuscript with support from Y.M.C and J.C.
All authors read and approved the final manuscript.
LIST OF ABBREVIATIONS
| IPL | = Intense Pulse Light |
| SSA | = Supramolecular Salicylic Acid |
| IPL | = Intense Pulsed Light treatment |
| IGA | = Investigator Global Assessment |
| BLT | = Blue Light Therapy |
| SPF | = Sun Protector Factor |
| PDT | = Photodynamic Treatment |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
The research protocol was approved by the institutional ethical review board of the first affiliated hospital of Chongqing Medical University (April 29, 2020, No. 2020-233).
HUMAN AND ANIMAL RIGHTS
No animals were used for studies that are the basis of this research. All the humans were used in accordance with the ethical standards of the committee responsible for human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2013 (http://ethics.iit.edu/ecodes/node/3931).
CONSENT FOR PUBLICATION
The written informed consent form was taken from the patients and volunteers.
STANDARDS OF REPORTING
STROBE guidelines were followed.
AVAILABILITY OF DATA AND MATERIALS
The data supporting the findings of the article is available in the Zenodo with title Efficacy of Supramolecular Salicylic Acid 30% Combined with Intense Pulsed Light Compare to Monotherapy Supramolecular Salicylic Acid 30% in Acne Vulgaris Patients at https:// zenodo.org/ record/ 7623652#.Y-SN1C-la-o, DOI: 10.5281/zenodo.7623652.
FUNDING
This study was supported by the National Natural Science Foundation of China (No. 81773307).
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
Declared none.
SUPPLEMENTARY MATERIALS
Supplementary material is available on the Publisher’s website.


