All published articles of this journal are available on ScienceDirect.
Unilateral Transverse Leukonychia in a Patient Receiving Isotretinoin Treatment with Concomitant Renal Impairment: A Case Report
Abstract
Aims:
Leukonychia is a white discoloration of nails. Although it is usually clinically insignificant, it can serve as a clue for systemic diseases that is sometimes life-threatening.
Case Report:
A 24-year-old male patient, with resistant acne vulgaris not responding to topicals nor systemic antibiotics and with a history of renal impairment and untreated recurrent high blood pressure readings, was started on isotretinoin. Three months later, he presented with a unilateral true transverse leukonychia with a worsening renal impairment. The patient was started on antihypertensive medications. The patient was seen two months later with unilateral transverse leukonychia fading (moving distally).
Results:
Repeated laboratory tests showed slightly increased serum creatinine, improved but still high protein/creatinine ratio. The fading of leukonychia while continuing isotretinoin treatment and after starting antihypertensive medication that has a renal protective effect may indicate a renal-associated leukonychia.
Conclusion:
This is probably the first reported unilateral leukonychia without identified local/unilateral causes.
1. INTRODUCTION
Leukonychia is a white discoloration of nails [1]. It is usually clinically insignificant and sometimes passed unnoticed [1]. However, it can serve as a clue for systemic diseases that is sometimes life-threatening [2, 3]. It is usually classified according to the morphological involvement of the nail, as total, partial, transversal, or longitudinal leukonychia [1]. True leukonychia is caused by a pathological process that starts in the nail matrix and proceeds to the nail plate [4]. It does not fade with pressure and moves distally with nail growth [4]. It can be a sign of numerous conditions, including trauma, neurovascular disorder, hereditary syndromes, systemic diseases, skin disease, hematologic disorders, toxicity with heavy metals, side effects of specific medications, and infection, and it can be idiopathic [1]. On the other hand, apparent leukonychia is caused by a pathology in the nail bed that is seen through the nail plate [4]. It fades with pressure and does not move distally with nail growth [4]. It can also be a sign of some systemic diseases, such as liver and renal diseases, a side effect of specific medications, and other conditions [1]. Here, we report a unilateral transverse leukonychia in a patient receiving isotretinoin treatment with concomitant renal impairment.
2. CASE REPORT
A 24-year-old male patient presented to the dermatology clinic with resistant acne vulgaris not responding to topicals or systemic antibiotics. The patient was started on isotretinoin 40 mg daily (0.5mg/kg/day), which was increased one month later to 60 mg daily. Three months after starting isotretinoin, the patient was seen at the dermatology clinic. He was complaining of headache and whitish discoloration of the nails of the right hand. The patient reported a history of intermittent high blood pressure readings over the last year, which was only treated by lifestyle modification. He also had a history of two abnormal creatinine levels over the last year. Moreover, he had recurrent gout attacks over the past two years, which required colchicine treatment. The patient reported no history of hand trauma nor a family history of renal disease. Further, the patient did not have any skin or nail manifestation suggestive of psoriasis.
On examination, the patient had unilateral transverse leukonychia over the right hand, sparing the thumbnail (Fig. 1). The whitish discoloration of the nails did not fade with pressure. The blood pressure reading was high (174/95 mmHg). Laboratory investigations revealed high serum creatinine (121 µmol/L), very high 24-hour urine protein (1216 mg versus the normal level of less than 150 mg), very high protein/creatinine ratio (1.93 versus the normal level of less than 0.20), high uric acid (721 µmol/L), and normal serum albumin (4.3 g/dL). Hemoglobin A1c (HbA1c), thyroid stimulating hormone (TSH), C-reactive protein (CRP), complement components 3 and 4 (C3 and C4), and potassium levels were normal. Autoimmune tests, including antinuclear antibodies (ANA) and antineutrophil cytoplasmic antibodies against proteinase 3 (PR3-ANCA) and myelperoxidase (MPO-ANCA), were all negative. Serum calcium and zinc levels were also normal. Potassium hydroxide examination for a sample from the proximal ventral nail plate and fungal culture to rule out proximal subungual onychomycosis were negative.
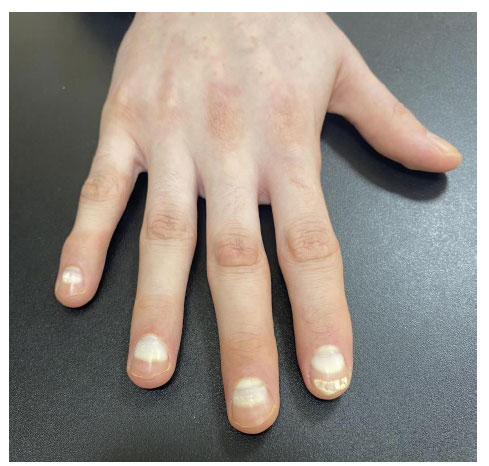
Doppler renal ultrasound showed normal findings. CT abdomen showed normal size and density of both kidneys with no calculi or hydronephrosis or perinephric fat stranding. It also showed a normal diameter of visualized upper ureters and unremarkable liver, adrenals, gallbladder pancreas, and lungs. The patient was referred to another hospital for an ultrasound-guided kidney biopsy. The patient was started on antihypertensive medications: a combination of an angiotensin-II receptor antagonist (irbesartan 150 mg) and a thiazide diuretic (12.5 mg hydrochlorothiazide) once daily. The patient was seen two months later with unilateral transverse leukonychia fading (moving distally, Fig. 2). Repeated laboratory tests showed slightly increased serum creatinine (134.1 µmol/L), improved but still high protein/creatinine ratio (0.51), and improved but still high uric acid (531 µmol/L).

3. DISCUSSION
We are reporting a unilateral transverse leukonychia in a patient receiving isotretinoin treatment with concomitant renal impairment. The current case represents a true leukonychia as it did not fade with pressure and moved distally with nail growth [4]. True leukonychia is postulated to be a result of abnormal matrix keratinization, with parakeratosis and keratohyaline granules causing light reflection and loss of transparency [1]. Being a unilateral leukonychia, the case is considered very rare. For example, unilateral leukonychia has not been reported before except in a few patients, after unilateral neurologic or neurovascular problems [5, 6] and after starting chemotherapy in a patient with metastatic breast cancer and same-side brachial plexopathy [7]. Leukonychia that affects some but not all fingers may also indicate local trauma or skin disease [1]. However, the current patient had no apparent neurologic or neurovascular problems and declined any history of trauma, and refused nail biopsy to rule out nail psoriasis.
Transverse leukonychia has been reported in association with numerous conditions, including systemic diseases and intake of specific medications [1]. However, transverse leukonychia is usually bilateral and affects almost all fingers [1]. For example, bilateral transverse leukonychia has been reported in association with isotretinoin [8] and acitretin [9]. Additionally, bilateral transverse apparent leukonychia has been reported in association with renal failure [10] and hypoalbuminemia [11]. Further, true leukonychia has also been reported in patients with renal diseases [1].
The current patient was on isotretinoin treatment for three months when the leukonychia was first diagnosed. Additionally, he had a history of recurrent high blood pressure readings and renal impairment. Although the latter could be aggravated by isotretinoin treatment [12], it was more likely to be caused by untreated hypertension. The current patient was not receiving other medications, and his blood pressure was managed by lifestyle modifications that were clearly not sufficient [13]. The fading of leukonychia while continuing isotretinoin treatment stands against the diagnosis of isotretinoin-induced transverse leukonychia. The fading of leukonychia after starting an antihypertensive medication that is also known for its renal protective effect [14] may indicate a renal contribution to the currently observed leukonychia.
Renal function tests were not done before starting isotretinoin treatment in the current patient and were not part of isotretinoin-required laboratory screening tests in our clinic. Similarly, they are not part of standard guidelines for baseline or repeated investigations for isotretinoin [15]. The current finding may not support their inclusion in baseline investigations for isotretinoin, given the rarity of isotretinoin-associated renal complications and the pre-existing disease in the current patient [12].
CONCLUSION
In conclusion, we have reported a unilateral true transverse leukonychia in a patient receiving isotretinoin treatment with a concomitant renal impairment. This is probably the first reported unilateral leukonychia without identified local/unilateral causes. The disappearance of leukonychia while continuing isotretinoin treatment and after starting antihypertensive medication that has a renal protective effect may indicate a renal-associated leukonychia.
LIST OF ABBREVIATIONS
| TSH | = Thyroid Stimulating Hormone |
| CRP | = C-reactive Protein |
| ANA | = Antinuclear Antibodies |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
Not applicable.
HUMAN AND ANIMAL RIGHTS
Not applicable.
CONSENT FOR PUBLICATION
Written informed consent form was taken from the patient.
STANDARDS OF REPORTING
CARE guidelines were followed.
AVAILABILITY OF DATA AND MATERIALS
The data that support the findings of this study are available within the article.
FUNDING
None.
CONFLICT OF INTEREST
The author has no competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
ACKNOWLEDGEMENTS
The author acknowledges the support provided by the Deanship of Scientific Research at Prince Sattam bin Abdulaziz University, Al-Kharj, Saudi Arabia.


