All published articles of this journal are available on ScienceDirect.
Dupilumab for a Novel Treatment for Necrobiosis Lipoidica: Case Report
Abstract
Background
This paper describes a case of necrobiosis lipoidica (NL) which was successfully treated with dupilumab. NL can be a difficult and chronic disease, often with limited treatment options. Dupilumab is a biologic typically used for atopic dermatitis, but given its novel pathway, it has been used in a number of other conditions.
Case Presentation
We describe a patient with inflammation on her legs, which was biopsied and consistent with NL. Treatments, including topical steroids, were started, but there was no improvement, therefore, dupilumab was discussed. She agreed with the treatment and dupilumab injections, and she reported a decrease in redness and improvement in her NL.
Conclusion
With this report, hopefully, there will be another option for the treatment of NL and different and novel uses for dupilumab.
1. INTRODUCTION
Necrobiosis lipoidica (NL) is a rare dermatologic granulomatous disease that is characterized by atrophic, erythematous plaques, typically on the lower extremities and manifests as a rash on the lower legs. NL is most often linked to diabetes metillus (DM), as it appears in 0.3% to 1.6% of diabetic patients, especially women and those who are insulin-dependent [1]. The symptoms of NL are in a constant state of flux, which chronically and unpredictably alternates between periods of agitation and suppression. In a state of flare, ulceration and telangiectasis frequently occur at affected sites, which causes itchiness, burning, pain, partial anesthesia, and discomfort in the area [2, 3]. The pathophysiology of NL is still unclear, but it is hypothesized to be a collagen dysfunction and/or autoimmune disease that leads to inflammation [1, 2]. The most successful treatments in the past, such as intralesional injection and topical introduction of corticosteroids, have been systemic, but the results have been short-lived and do not address the chronic nature of the disease. Moreover, the prolonged administration of steroids could disrupt the body’s regulation of fluids and result in worsening high blood pressure in diabetic patients [2, 4]. What is unique to this case is that we report a case of persistent and refractory NL that was successfully treated with dupilumab, which has not been reported in the literature.
2. CASE PRESENTATION
A 71-year-old female with no other medical history was presented with erythematous, sensitive plaques that encompassed most of her legs (Fig. 1). A biopsy was performed and results were consistent with NL (Fig. 2). Tacrolimus and betamethasone dipropionate ointment were used without any improvement. The patient continued to report redness and pain in the areas on her legs, not improving with topical therapy. Given her age, oral steroids were withheld, given possible side effects. She denied having a history of diabetes; however, the biopsy was indicative of NL, which can be present without concurrent DM.

Patient presenation of NL prior to treatment with dupilumab.
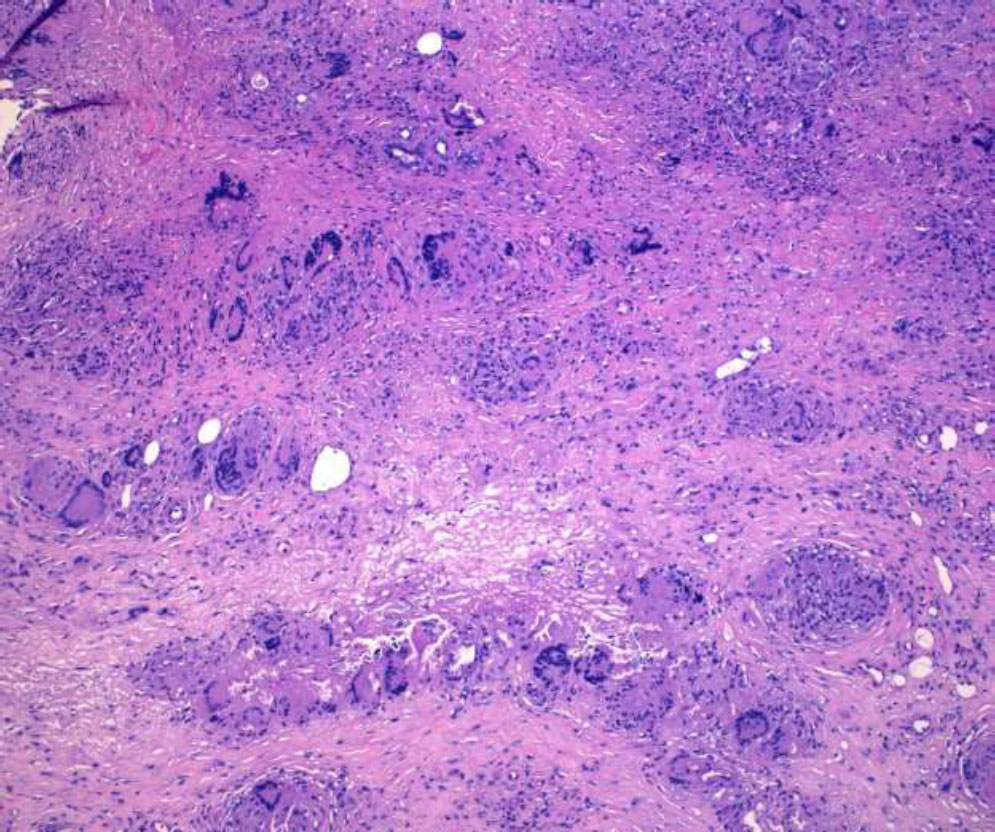
Histopathology of punch biopsy showing NL.
Given the recalcitrant nature of her condition, along with the relative safety of dupilumab, treatment with dupilumab injections was suggested. After further discussion, the patient agreed to perform a trial of dupliumab injections for two months. A dose of dupilumab 600 mg was administered subcutaneously in the abdomen. Remarkably, only after two weeks her NL significantly improved (Fig. 3). Given her improvement, topical steroids and tacrolimus were discontinued. After her first dose, the patient was kept on 300mg every 2 weeks with no adverse side effects from the therapy. She continued to be well-controlled for four months on dupilumab. The inflamed plaques on the patient’s calves now appeared as post-inflammatory hyperpigmentation. Despite significant improvement, the patient remained on dupilumab due to small residual inflamed areas around the ankles. Furthermore, the patient reported that her symptoms had improved, including burning and irritation in her lower extremities. She used her topical steroid, betamethasone dipropionate cream, sparing a few active areas, but her use and amount had been greatly diminished given the use of dupilumab.

Improvement of NL after treatment with dupilumab.
3. DISCUSSION
Necrobiosis lipoidica (NL) is a rare dermatologic condition which manifests as a rash characterized by slow healing, red, yellow, and brown lesions due to dermal collagen degradation and decreased collagen synthesis [5]. NL is most oftenly linked to diabetes metillus (DM); however, patients can develop NL without a history of DM, such as our patient. The pathophysiology of NL is hypothesized to be due to an immune-mediated vascular disease leading to collagen dysfunction and inflammation [4, 5]. The most successful treatments in the past have been systemic, intralesional injection, and topical corticosteroids, but the results have been short-lived.
Dupilumab (dupixent) is an interleukin-4 (IL-4) receptor alpha antagonist, which blocks the signaling pathway of IL-4 and interleukin-13 (IL-13) [6]. IL-4 is a T-cell-derived cytokine that participates in brain functions such as memory and learningi. When IL-4 in the cerebrospinal fluid (CSF) interacts abnormally with the brain, it is often associated with autoimmune attacks and other immune-related conditions [7]. Thus, IL-4 plays a significant role in autoimmune conditions and in our case, both NL and atopic dermatitis fall into that category. Having both overlaps with IL-4 may help explain the relationship with dupilumab in both conditions. IL-13 functions cooperatively with IL-4 and plays a large role in the regulation of B cells and monocytes, specifically in the allergic asthma response [8]. The mechanism of dupilumab inhibits IL-4 and IL-13 signaling to prevent unwanted cytokine-induced responses, such as the release of proinflammatory cytokines, chemokines, and immuno- globulin E (IgE), which contribute to abnormal immune activation [9]. Through this mechanism of action, dupilumab has been successful in treating a variety of immune-related conditions, such as atopic dermatitis, asthma, and chronic rhinosinusitis [8]. Therefore, dupilumab is a relevant treatment option for NLD, which is categorized as an inflammatory immune condition based on abnormalities in T cells [10]. Dupilumab also blocks the signaling of IL-13. IL-13 is important in type 2 inflammation [6]. Decreasing the drivers of type 2 inflammation may help decrease the positive feedback that occurs in autoimmune diseases, explaining its role in AD and possibly in NLD.
CONCLUSION
This case report exhibited a 71-year-old female who was confirmed to have NL through biopsies and did not benefit from topical therapies, such as tacrolimus and betamethasone ointments. Upon treatment with dupilumab, the chronic plaques on her lower legs improved within two weeks of the treatment start date. These results suggest that the pathology of NL may rely on IL-4 and IL-13, which can be successfully targeted by dupilumab. However, clinically in our patient, we noticed marked clinical improvement on dupilumab. It would be interesting to discern the effect of dupilumab on NL and whether it is the IL-4 pathway or IL-13 pathway which addresses the main pathology of NL. However, it is possible it could be a combination of the two. By publishing this report, hopefully, other providers would be able to take interest and also try this novel and safe treatment on other patients who are diagnosed with NL.
AUTHORS’ CONTRIBUTION
It is hereby acknowledged that all authors have accepted responsibility for the manuscript's content and consented to its submission. They have meticulously reviewed all results and unanimously approved the final version of the manuscript.
LIST OF ABBREVIATIONS
| NL | = Necrobiosis Lipoidica |
| DM | = Diabetes Metillus |
| CSF | = Cerebrospinal Fluid |
| CSF | = Cerebrospinal Fluid |
| IgE | = Immuno-globulin E |
AVAILABILITY OF DATA AND MATERIAL
The data supporting the findings of the article is available in the Zenodo Repository https://zenodo.org/re cords/14523599?preview=1&token=eyJhbGciOiJIUzUxMiJ9.eyJpZCI6IjJiMjVlNDE0LWY2NzYtNGFhMi1hOTg0LThmYmFjZmY3YzlhYiIsImRhdGEiOnt9LCJyYW5kb20iOiJjZmU0NzFmMzFjNmNjYjY2MzRjY2VhMGQ0YzJlZmMzMyJ9.wERN20t6c8XNaTxuDylE5mexzLiRHrmfhfnjRoKHey9-6wsYjCZ-F3eOCUqUGXBO2c_K4wUnX68qsvLpHmNmXA


