All published articles of this journal are available on ScienceDirect.
The Role of Dermoscopy in Assessment of the Activity and Scarring Response in Discoid Lupus Erythematosus
Abstract
Background:
The diagnosis of Discoid Lupus Erythematosus (DLE) is usually made by clinical examination and by histopathology. Recently, dermoscopy has become an integral part in diagnoses of many inflammatory disorders and one of these is DLE.
Aims:
This research emphasizes the utility of dermoscopy in the assessing lesions of DLE from the point of activity of the disease.
Patients and Methods:
Thirty-one patients diagnosed with DLE were included in this study. The total number of examined lesions was 125 lesions. All of the lesions were assessed by dermoscopy at different stages of the activity of the diseases.
Results:
The dermoscopic features of DLE vary according to the stage of activity of the disease. There are characteristic dermoscopic features for the lesions of the scalp different from that of the body. In the active and early phase, the most common dermoscopic features were the presence of lesional and perilesional scales, follicular keratotic plugging, telangiectasia, arborized blood vessels, follicular red dots and perifollicular scales. In addition, there are less common dermoscopic features such as pigmentary changes, white rosettes and pinpoint white dots. For active scalp lesions, the follicular plugging and perifollicular scales were more prominent than that of the body DLE lesions. For inactive and late DLE lesions, the most significant dermoscopic changes were perifollicular whitish halos, variable patchy whitish hypopigmented areas, and the presence of white colored structureless areas.
Conclusion:
The present study provides new insights into the dermoscopic variability of DLE lesions at different levels of activity.
1. INTRODUCTION
Discoid Lupus Erythematosus (DLE) is the chronic form of the cutaneous type of lupus erythematosus [1]. It represents the most common subtype of cutaneous lupus erythematosus, and commonly affected females [2]. It may occur at any age, but most frequently at middle age. This is a scarring disease that can cause permanent scarring if treatment is inadequate or ineffective. Patients with DLE are often divided into two subtypes: localized (lesions occur only on the head or neck) and generalized (occurs below the chin with or without lesions present above this level). Clinically, the DLE patients present with a fairly defined, erythematous patches and plaques with adherent scale. Early lesions present as a well-demarcated round or oval purplish macule or papule with little scaling. By the time, some of these lesions progress to annular lesions that enlarge into a patch with follicular plugging, erythema, and adherent scaling. The old and end-stage disease is characterized by fibrotic and atrophic patches that may be hypo- or hyperpigmented without follicular ostia. Scarring alopecia occurs in the scalp and other hairy areas in about one-third of patients and is usually permanent [3, 4]. The diagnosis is based on direct immunofluorescence, and histopathology [5]. By histopathology, early DLE showed prominent perivascular and periadnexal lymphohistiocytic, an interface dermatitis, basal layer degeneration, and marked thickening of the basement membrane. In well-established lesions, there may be marked follicular plugging and acanthosis.
Recently, dermoscopy has become an integral part of diagnosing many inflammatory disorders [6] and one of these is DLE. It is very helpful in the diagnosis of various general dermatological disorders, including scalp/hair diseases [7]. It has been shown to be an effective tool to differentiate the scalp DLE from other causes of scarring alopecia such as lichen planopilaris [8]. In addition, there were reports [9-14] documented specific dermoscopic features of DLE in other locations, such as the face. These features included follicular plugging, telangiectasias, arborizing vessels, honeycomb pigmented network, variable scaling, and perifollicular whitish halo. Also, rosettes and structure-less white and brown areas have been reported by others [13, 14]. All of the previous dermoscopic features were correlated well with histopathological findings.
This research emphasizes the utility of dermoscopy in the assessing lesions of DLE at different stages of activity. Dermoscopy may be a good tool in assessing the lesions of DLE at different stages of the activity of the disease (active and new lesions, active edge of old or new lesions, perilesional skin, and old scarred lesions.). In addition, it will be a good way to follow up the patients with DLE and to assess the response to treatment. Patients with discoid lupus erythematosus diagnosed initially by histopathology and immunofluorescence, and they are followed up and assessed subjectively by clinical features. Dermoscopy may help in making follow up for these cases by objective means looking for features of activity of the disease. In addition, the previous reports published on dermoscopy of DLE lesions in the past few years, have been mainly carried on western countries and Indian population. The patients of the study were from Jordan (one of the Arab Middle East countries).
2. PATIENTS AND METHODS
This was an out-patient clinic-based study done in dermatology clinics (Mutah University Medical Center, Jordan) from January 2015 to April 2018. The ethical committee approved the study protocol. Informed consent was obtained from the patients before enrolment in the study.
All patients diagnosed with discoid lupus erythematosus (based on clinical, physical and histopathological examinations) were included in this study. All DLE lesions located on the scalp, face, trunk, and extremities were examined by dermoscopy. The intention was to examine DLE lesions at a different stage of activities: active and new lesions, active edge of old or new lesions, perilesional skin, and old scarred lesions. A dermoscopic examination of all cases was performed using a hand-held dermoscope (Dermlite DL3, Gen, USA) application which captured images with iPhone, and then was evaluated as saved photos on a computer screen. This dermoscopy can block light reflection from the skin surface without immersion gels or alcohol. The Characteristics and specifications of the DermLiteDL3 dermoscope used in the study were 20x and 40x magnification with focusing optics. The dates and times of capturing photos were automatically stored. Selection of the dermoscopic variables included in the evaluation process was based on data in the available literature on DLE of the scalp and our preliminary observations.
3. RESULTS
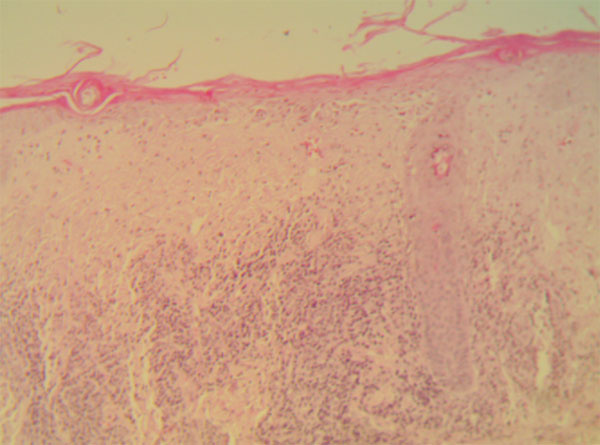
Thirty-one patients diagnosed with DLE were included in this study. All of the patients were diagnosed clinically and confirmed by histopathological means (Fig. 1). Four of the cases were males with a mean age of 34 years. The females were with a mean age of 28 years. Two of the cases (males) had exclusive scalp involvement. 29 of cases had mixed scalp and body involvement by discoid lesions. Three cases (females) has generalized DLE. The total number of examined lesions by dermoscopy was 125 lesions from 31 patients. The clinical data were summarized in Table 1.
All of the DLE lesions were assessed clinically and dermoscopically at different stages of the activity of the diseases (active and new lesions, active edge of old or new lesions, perilesional skin, and old scarred lesions). Clinically, the active DLE lesions of the scalp were characterized clinically by being indurated erythematous plaques with slight scales. These scales were mild, adherent, and some were perifollicular. Follicular plugging was a common finding in most of the scalp lesions; these plugs were more pigmented in patients with skin type IV. The marginal skin was indurated and erythematous. The perilesional skin was slightly more erythematous. Older lesions in the scalp were scarred with central loss of pigmentation (white patches), atrophic, and with loss of hair ostium. Some of the edges of plaques showed marginal hyperpigmentation especially in older lesions (Fig. 2).

| Clinical Data | ||
| 1. | Number of the patients | 31 patients |
| 2. | Sex | 4 males and 27 females |
| 3. | The mean age | males (34 years) females (28 years) |
| 4. | The clinical types of DLE | Two cases had exclusive scalp lesions 29 cases had mixed scalp and body DLE lesions |
| 5. | The total number of examined DLE lesions | 125 lesions were examined by dermoscopy |
| 6. | The scalp DLE lesions | 56 were active lesions 13 were old and inactive lesions |
| 7. | DLE lesions on the body | 40 were active lesions 16 were old and inactive scarred lesions |
Similarly, the presentation of active lesions of the DLE of the body (including face, trunk, and extremities) was as an erythematous papule or plaques with slight-to-moderate scales (Fig. 3a). Some of the lesions showed more thickened and adherent scales. The active edges were more indurated and erythematous compared to the perilesional skin which also showed some erythema. The older lesions were atrophic and sclerotic. These burnt-out DLE lesions were commonly hyperpigmented (Fig. 3b).


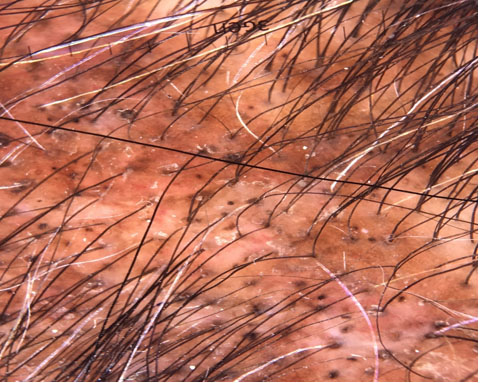
Dermoscopically, the presence of keratotic follicular plugging was a common finding especially in active and early DLE lesions of the scalp; they have been seen in 52 lesions (93%) of DLE. They have been observed in active DLE lesions from the face and trunk but to a lesser degree (22 lesions (55%)). These keratotic plugs appeared as dark yellow-brown dots and were very numerous from scalp lesions compared to these from face or trunk (Fig. 4). These follicular pluggings have been seen uncommonly in four old inactive scalp DLE lesions (31%) and two inactive lesions facial lesions (13%). For older lesions, these follicular plugging was replaced with follicular whitish halo (Fig. 5) with lost hair ostium and loss of follicular opening. This had been observed in all old scarred lesions from the scalp and body and occasionally from 6 active lesions of the scalp (11%) and four lesions from the trunk (11%).

Clinically the active DLE characterized clinically as erythematous lesions, and this has been observed dermoscopically by the abundance of the lesional and perilesional telangiectasia and thick branching blood vessels (Fig. 6). This has been seen in 50 active DLE lesions of the scalp (89%), and with similar frequency from 38 lesions from face and trunk (95%). Even in old and scarred lesions, these arborized blood vessels have been seen but at a lesser degree and more blurred (60% of the scalp and 50% from the face and trunk).

It has been common to see the scaling in new and active lesions, these have been diffuse within the plaques of DLE (Fig. 7a). This was seen in all new active lesions of the scalp, face and truncal lesions. The active edges also demonstrated these scaling and in the perilesional skin. For old and inactive lesions, these scales were seen only in perilesional skin and at the active edge. Particularly, in the active scalp lesions, some hair follicular demonstrated perifollicular scaling (42 lesions (75%)), these were occasionally seen from nine lesions of body DLE (23%) (Fig. 7b).

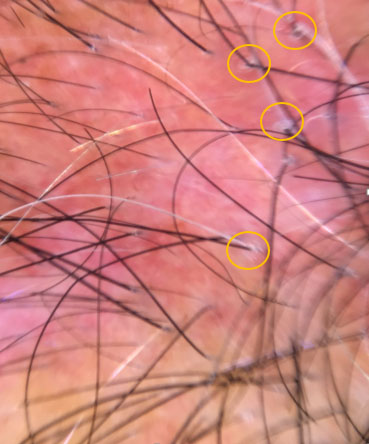
Follicular red dots were a common finding in active DLE; it has been seen in 37 lesions (66%) and 70% of facial lesions (12 lesions). They appear as an erythematous and concentric structure around the hair follicle (Fig. 8). These are non-exclusive in new lesions; as has been in some scarred lesions (6 lesions from the scalp and body).

Pin-point white dots (Fig. 9) were another common dermoscopic features; they are white dots distributed throughout the plaques of DLE lesions between hair follicles. This was a common finding in 37 active scalp lesions (66%) and 28 body lesions (70%). They appear smaller than these of whitish halos which surrounded the hair follicles. In addition, it has been seen in the perilesional skin of some old DLE lesions of the scalp (38%) and facial skin (38%).
White rosettes were another but uncommon dermoscopic features in the patients of the study. These were shiny white structures seen as four oval-shaped points that come together in the center. They had been observed in only three active lesions of scalp DLE but was more common from DLE of the trunk and face (10 lesions). They have also been seen even in old hyperpigmented lesions especially in old scarred lesion especially from the trunk (4 lesions) (Fig. 10).
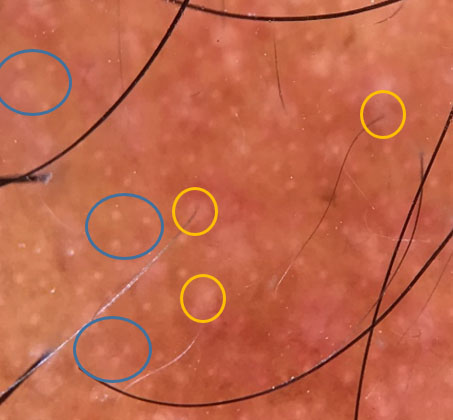

Pigmentary changes (Fig. 11) in DLE lesions were common, especially in old inactive lesions. Patchy honey comp pigmentations were seen in 19 active scalp lesions (34%). Perifollicular hyperpigmentation was seen in 8 active scalp DLE lesions (14%). Regarding the old and scarred lesions, the most characteristic finding was follicular whitish halo and variable patchy whitish hypopigmented areas. The margin of these plaques was hyperpigmented. Similar pigmentary changes were recorded from active DLE of the face and trunk as scattered dark-brown pigmentations in active lesions (55%). Old lesions of body DLE (16 lesions) characterized by the presence of white colored structureless areas, hyperpigmentation in the form of a honeycomb network, and blurred telangiectasia. These dermoscopic features were seen characteristically in all old discoid lupus erythematous lesions.
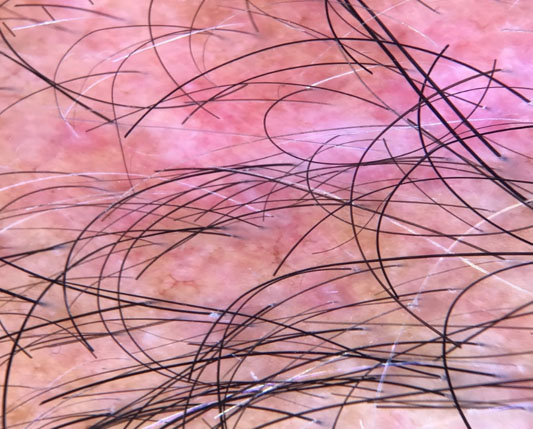
Table 2 summarized all of these dermoscopic features in active and old scarred DLE lesions.
| Dermoscopic Feature |
Active Scalp DLE Lesions No of Lesions =56 |
Inactive and Old Scalp DLE Lesions No of Lesions =13 |
Active DLE Lesions (Face, Extremities, and Trunk) NO of Lesions =40 |
Inactive and Old DLE Lesions (Face, Extremities, and Trunk) No of Lesions =16 |
|---|---|---|---|---|
| Follicular keratotic plug | 52/56 (93%) Vey numerous, yellow-dark brown |
4/13 (31%) Few in numbers, more keratotic |
22/40 (55%) Numerous, Yellow in color |
2/16 (13%) Few in numbers, more keratotic |
| Follicular whitish halo | 6/56 (11%) Very few |
13/13 (100%) Numerous |
7/40 (11%) Very few |
16/16 (100%) Numerous |
| Telangiectasia and arborized blood vessels | 50/56 (89%) Lesional and perilesional |
8/13 (60%) The blood vessels and telangiectasia more blurred |
38/40 (95%) Lesional and perilesional |
8/16 (50%) The blood vessels and telangiectasia more blurred |
| Scales | All of lesions (lesional and perilesional) | prominent at the active edge of all lesions | All of lesions (lesional and perilesional) | prominent at the active edge of all lesions |
| Perifollicular scales | 42/56 (75%) | Occasional One case |
9/40 (23%) | None of the cases |
| Follicular red dots | 37/56 (66%) | 3 lesions (23%) | 28/40 (70%) | 3 lesions (19%) |
| Pin-point white dots | 34/56 (61%) In the lesional and perilesional skin |
5 (38%) In the perilesional skin |
28 (70%) In the lesional and perilesional skin |
6 (38%) In the perilesional skin |
| White rosettes | 3/56 (5%) | 1 lesion (8%) | 10/40 (25%) | 6 (38%) |
| Pigmentary changes | Patchy honey comp pigmentations were seen in 19 lesions (34%). Perifollicular hyperpigmentation was seen in 8 lesions (14%). |
Follicular whitish halo, Variable patchy whitish hypopigmented areas. The margin of these plaques was hyperpigmented. |
Scattered dark-brown pigmentations in 22 active lesions (55%) | Presence of white colored structureless areas, Hyperpigmentation in the form of a honeycomb network, |
4. DISCUSSION
DLE is a chronic inflammatory disease with liability to scar formation. The lesions of DLE develop initially as erythematous-to-violaceous, inflamed papules and patches with crusting and scaling appearance. Follicular plugging is a common feature in these early and active lesions. Later on, the center of these patches or plaques may appear lighter in color, that often results in scarring and atrophy with an edge darker than the normal skin. When lesions occur in hairy areas such as the scalp or beard area, permanent scarring and hair loss can occur.
Early recognition and treatment improve the prognosis [15]. This current report documents the dermoscopic features in DLE at different stages of disease activity. The aim was to describe dermoscopic criteria observed in a series of patients with DLE had their lesions on the scalp and body, at active and inactive disease activity. The patients of the study were from Jordan (one of the Arab Middle East countries). The skin type of the patients of the study was mainly with a Fitzpatrick skin type of III and IV. The previous reports published on dermoscopy of DLE lesions have been mainly carried on western countries and Indian population.
Thirty-one patient with DLE (diagnosed clinically and by histopathology) were examined by dermoscopy. The total number of the lesions was 125 (including active, inactive and old scarred lesions from scalp and body (trunk and extremities)). Clinically, active and new lesions from the scalp and body look similar. All lesions were erythematous and indurated plaques. Scales were prominent in the lesional and perilesional skin and mainly perifollicular in scalp lesions. In addition, follicular plugging was a common finding in lesions from the scalp and hairy areas; they are darker in patients with skin type IV than those of type III. Older lesions in all sites were scarred with central loss of pigmentation (white patches), atrophic, and with loss of hair ostium. The marginal skin was indurated and erythematous. In addition, some lesions showed hyperpigmented pigmentary changes that developed within the old scarred patches and at the active borders.
The dermoscopic features in DLE vary according to the stage of activity of the disease. In addition, there are characteristic dermoscopic features for the lesions of the scalp. The results showed that different dermoscopic features were seen according to the localization of DLE lesions, disease duration and the activity of the disease. In the active and early phase, the most common dermoscopic features were the presence of lesional and perilesional scales, follicular keratotic plugging, telangiectasia and arborized blood vessels, follicular red dots and perifollicular scales. In addition, there are less common dermoscopic features such as pigmentary changes, white rosettes and pinpoint white dots. For active scalp lesions, the follicular plugging and perifollicular scales were more prominent than that of the body DLE lesions. For inactive and late DLE lesions, the most significant dermoscopic changes were perifollicular whitish halos, variable patchy whitish hypopigmented areas and the presence of white colored structureless areas. The active edge of these latent lesions showed blurred telangiectasias and marginal hyperpigmentation.
The most common dermoscopic features for early and active DLE lesions was the presence of scales (lesional and perilesional skin). This was a common feature for all DLE lesions from the scalp and body. For old and inactive DLE lesions, these scales were localized at the active edge and perilesional skin. The presence of the scales at the perifollicular areas was a common and characteristic feature for active DLE from the scalp; it had been seen in two-thirds of cases compared to active lesions from face and body which had been seen in 23% of cases. In addition, this perifollicular scaling was absent from all inactive and old lesions of DLE from the scalp or body; so it can be considered as a sign of activity of the disease.
Follicular plugging was another common and important dermoscopic features of DLE lesions from the scalp (93%) of lesions. They were numerous and yellow to dark brown in color. It has been observed but to a lesser degree from the facial and body lesions (55%). Follicular keratotic plugs were considered as a marker of DLE [16] and correlate with the hyperkeratosis and plugging of the follicular ostia with a keratotic material. And this is expected in a disease like DLE in which the process of inflammation targets the skin and follicular structures [17]. For old and inactive lesions from the scalp and body, the follicular plugging was uncommon finding. They have been replaced by fibrosis and this was seen dermoscopically as follicular whitish halos which has been seen in all of inactive and scarred DLE lesions from the scalp and body and occasionally in inactive lesions (11%). The presence of these halos can be considered as a characteristic feature for a late and inactive disease.
Characteristically, the active lesions of DLE are erythematous one, even for late and inactive lesions. The margins are red and the perilesional skin more erythematous than uninvolved skin. This was visualized dermoscopically in all lesions as lesional and perilesional telangiectasia with the presence of thick arborizing vessels even at the margin of old and late lesions. These vessels are significantly wider than that of arborizing vessels in the normal scalp or seborrheic dermatitis [18, 19]. These vessels were seen similarly in indistinguishable from those in basal cell carcinoma. This vascular network, which is visible through the thinned atrophic epidermis may explain the milky red (pink) fibrosis that seen in DLE fibrotic lesions and not as an ivory white, as in most other types of cicatricial alopecia. This results from the vascular network, which is visible through the thinned atrophic epidermis [19].
A novel dermoscopic feature observed in DLE by Tosti et al. [12]. was a red follicular pattern and was considered as a specific feature of scalp lesions of active lupus erythematosus of the scalp. These dots correspond to widened infundibula with dense perivascular lymphocytic in filtrates, dilated vessels, and extravasated erythrocytes [11, 20]. The loss of this pattern in DLE may be a sign of hair follicle damage with poor prognosis [20]. Recognition of this distinctive dermoscopic pattern may help the clinician to differentiate DLE from other diseases causing cicatricial alopecia [12] . This has been in the patients of this study as multiple red dots, which are regularly distributed in and around the follicular ostia. This has been seen nearly in two third of active lesions of DLE from the scalp and body. It was seen uncommonly in few inactive lesions. Their presence in these old lesions may be associated with a good prognostic factor for hair regrowth [12].
Another feature was seen in active DLE lesions of this study was the presence of dark-brown discoloration of the skin in both DLE lesions from the scalp and body. The localization and distribution of melanin and haemoglobin pigment in skin layers reflect these characteristic patterns of altered pigmentation which is visualized using dermoscopy [21]. This finding corresponds to pigment incontinence on histopathology [22]. Dark brown to blue-grey pigment pattern is seen in DLE affecting the interfollicular area unlike in LPP where it is concentrated around the follicles. For longstanding inactive DLE lesions, the prominent pigmentary change was the presence of presence of structureless pink or white areas and follicular whitish halos. The hyperpigmentation was seen mainly at the advancing active edges.
A new report of white rosettes in discoid lupus erythematosus has been reported recently [13]. They are shiny white points seen under polarized dermoscopy. They vary in size from 0.2 mm to 0.5 mm, and they can be oriented in the same or in different angulations [23]. Many authors believe that it is due to the optical effect of polarized light. It is postulated that rosettes are formed by narrowing of infundibula or blockage by keratin [24]. Others suggested that rosettes correspond to an alternating focal hyperkeratosis and normal corneal layer and keratin-filled acrosyringeal openings. These rosettes were occasionally seen in this study; only a few lesions of active DLE lesions, but seen more in old and latent DLE lesions of the body (38%). The rosettes may be may be attributed to concentric perifollicular fibrosis. White rosettes are not specific dermoscopic patterns to any particular condition as has been seen in other types of scarring alopecia and skin diseases [23, 24]. In addition to these whitish rosettes, there were pin-point whitish dots distributed through the lesional and perilesional DLE patches and plaques. They have been seen in all lesions but to a lesser degree than latent lesions. These represent the opening of eccrine glands and are not specific for DLE as has been described in other types of scarring alopecia and in normal scalp [25, 26], so they are not specific for DLE nor the activity of the disease.
The above dermoscopic features of DLE lesions may reflect the dynamic process of the disease its self. There were specific features indicated the activity of the disease and were seen to a lesser degree as the disease became more late and inactive. There were some features that can be considered as specific if combined with other dermoscopic features such as the presence of keratotic follicular plugging and erythematous follicular dots within a background of lesional telangiectasia and scales. Some of the dermoscopic features were not specific such as rosettes sign and pinpoint white dots. Presence of perifollicular white halos may be an impending sign of progression of the disease to a fibrosis and scar formation. The present study provides new insights into the dermoscopic variability of DLE located on the face, trunk, and extremities at different levels of activity of the disease.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
This study has been approved by the Research Ethics Committee of Mutah University.
HUMAN AND ANIMAL RIGHTS
No Animals were used in this research. All human research procedures followed were in accordance with the ethical standards of the committee responsible for human experimentation (institutional and national), and with the Helsinki Declaration of 1975, as revised in 2013.
CONSENT FOR PUBLICATION
A written informed consent was obtained from all patients when they were enrolled.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
Declared none.


