All published articles of this journal are available on ScienceDirect.
Effects of Corona Virus on the Skin: Symptoms and Risks
Abstract
Coronavirus is a disease that affects mainly the upper respiratory tract, but in somecases, it can also affect the skin. This study aims to describe the effect of coronavirus on the skin function. Skin gets affected easily because coronavirus first comes into contact with the skin and mucous membrane. Numerous studies are investigating the symptoms of coronavirus appearing on the skin in different forms like rashes, blisters, irritation, dermatitis, etc. The excessive use of sanitizers and soaps can also cause skin problems. Personal protective equipment can also cause irritation to the skin and mucous membrane. It is concluded from the study that skin must be protected from the exposure of the external environment where the virus may be present. Moreover, sanitizers and soaps must be used in a limited quantity and proper medication should be taken by the patients having a skin disease because they may get affected with the coronavirus.
1. INTRODUCTION
An outbreak of coronavirus disease 2019 (COVID-19), caused by a novel extreme acute respiratory coronavirus 2 syndrome (SARS-CoV-2), occurred in Wuhan City, Hubei Province, China in early December 2019. The epidemic was declared a Public Health Emergency of International Concern by the World Health Organization on 30 January 2020. Forty-nine thousand fifty-three laboratories confirmed the cases of COVID-19 with 1,381 deaths on 14 February 2020. The cases started being reported from 8th December 2019, including several patients working or living in the local Huanan Seafood Wholesale Market [1]. This virus belongs to the family β-coronavirus, a broad class of viruses prevalent in nature. SARS-CoV-2 has several possible natural hosts, intermediate hosts and end hosts, similar to other viruses. This poses major challenges for the treatment of viral infections. Compared to extreme acute respiratory syndrome and coronaviruses of the Middle East respiratory syndrome (SARS-CoV and MERS-CoV), SARS-CoV-2 has high transmissibility and infectivity and low mortality rates. Genome review of SARS-CoV-2 sequences shows that the complete genome sequence recognition rates of SARS-CoV and bat SARS coronavirus (SARSr-CoV-RaTG13) are 79.5% and 96%, respectively [2].
Some COVID-19 patients have shown aggravation of prior skin disorders such as rosacea, eczema, atopic dermatitis and neurodermatitis. Due to prolonged use of masks during the epidemic, facial acne and rosacea occurred or aggravated. Frequent use of skin disinfectants has increased the incidence of contact dermatitis not only in patients with COVID-19 but also in healthy individuals and medical personnel. Many dermatologists in China are opening free online consultations to give support to the people. During the epidemic, specific treatment methods should be considered for some skin diseases. People with multiple skin disorders such as psoriasis are at higher risk of developing cardiovascular disease, depression and other health problems that may increase the occurrence of serious cases and death following COVID-19. Therapeutic drugs such as IL-17 inhibitor, which rapidly regulate skin lesions and have lower effects on immune functions compared to conventional immunosuppressants, may be considered as first-line therapy in the current situation. It is also based on some claims that some biological agents could be useful in treating novel coronavirus pneumonia, although the therapeutic efficacy of biological agents in both skin diseases and novel coronavirus pneumonia is still under the clinical research stage [3].
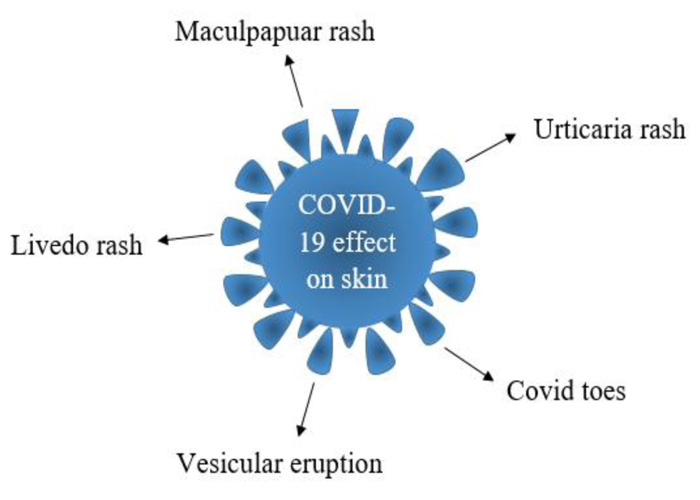
Numerous cases of skin rashes in COVID-19 patients are spreading across the globe. The rashes can take many forms; some of them appear as tiny red spots while others appear as larger flat or raised lesions. Some have hive-like appearance, while others look like frostbitten feet. According to a Spanish research, skin eruption related to coronavirus is categorized into five types including ‘maculpapuar’ rash, or one that is typical of viral infections such as measles, with red bumps on reddish skin, a hives related ‘urticaria’ rash, a lace like or fishnet pattern ‘livedo’ rash, a ‘vesicular eruption’ or blistering rash and frostbite like a rash on toes, unofficially dubbed ‘covid toes’ [4]. Fig. (1) shows the schematic diagram of the five types of skin-related symptoms that appeared after the COVID-19 infection.
2. SKIN RELATED PROBLEMS CAUSED BY COVID-19 VIRUS
A report on the effect of the coronavirus on dermatology, authored by a group led by Juan Tao, the dermatologist from Huazhong University of Science and Technology, was published in the British Journal of Dermatology. The author’s team suggested that the dermatological conditions of the skin may result in an increased risk of infection by the novel coronavirus (2019-nCoV). Dr. Tao summarized the theoretical risk of coronavirus. They also discussed that coronavirus might cause skin infection through contact with subcutaneous tissues, mucosal surfaces or blood vessels. However, Adam Friedman, a professor of dermatology at George Washington University, Washington, said that he doubts that any such transmission would occur because of the virus; it does not infect keratinocytes of the skin. He expressed concerns about the disgrace felt by dermatological patients, whose visible rashes can often lead to social avoidance [5].
According to the WHO, the use of bleach or other disinfectants on the body does not protect from COVID-19. Bleach or any other disinfectant is poisonous if ingested and causes irritation and damage to the skin. The hands must be cleaned by alcohol-based hand washor washing hands with a gentle soap and water is the most easily applicable way to remove the virus. Ultra-violet lamps cannot be used to disinfect the hand or different areas of the skin as it may cause skin irritation [6].
An Italian physician, in late March, describes the skin conditions that occur due to coronavirus. According to the physician, 20% of 88 patients showed symptoms of red rash on their torsos and few suffered from hives or blisters like in chickenpox. Another study result was reported in early April by a dermatology organization, representing more than 400 French dermatologists; they all stated that the patients of coronavirus had some symptoms related to skin such as red rashes, hives and frostbite like lesions [7, 8].
Tursen et al., have described the skin problems such as erythematous rash, urticarial, petechial and vesicles in 20% of coronavirus patients. In most of pediatric coronavirus patients, vascular and vasculitic skin changes such as purpura, petechiae, livedoid and ecchymosis lesions have been also observed. Coronavirus may show signs of a small occlusion of blood vessels, such as tiny bruises or petechiae and transient unilateral livedoid eruptions. Coronavirus has been found to attack the β-chain of hemoglobin and captures porphyrin to block the synthesis of heme. This result can explain the vascular changes of the skin because of coronavirus. It was also observed that medical masks could induce rosacea, acne vulgaris, erosions and ecchymosis of skin [9].
According to Doctor Misha Rosenbach from the University of Pennsylvania, the patients infected with coronavirus named as COVID toes by the dermatology community. The toes and fingers have discoloration of red and purple color, which may be a symptom of coronavirus. Other skin conditions have also been reported, such as measles, hives or rashes. In another study Doctor Joanna Harp reported that skin conditions such as the pattern of lacy, dusky rashes and dead skin cells on the arms and legs may be caused by coronavirus [10].
Skin rashes have been commonly found in coronavirus patients, and other problems related to the skin are described such as an erythematous exanthaem (including lacy pattern and a petechial, dengue like rash), livedo reticularis, cutaneous vasculitis, acute urticaria, chickenpox like blisters and COVID toes that are also described as pernio or chilblains or frostbite [11].
While the virus is not dermatotropic, some skin disorders have arisen, primarily due to prolonged contact with personal protective equipment and excessive use of personal hygiene products. Darlenski et al., described the pressure infection, hives, itching, contact dermatitis and exacerbation of pre-existing skin diseases, including acne and seborrheic dermatitis problems caused by coronavirus. Eventually, mucosal membranes have been recognized as the common medium of carrying the infection, including the conjunctiva with the octic canal having less transmission risk. Complications of the skin in coronavirus mainly occur due to the hyper-hydration effect of personal protective equipment. These equipment can cause the breakdown of the epidermal barrier, contact reaction and friction, which may exacerbate an already established skin problem. Papules, scaling, maceration and erythema are the adverse effects on skin most frequently recorded due to prolonged wear of personal protective equipment. The symptoms observed include itching, stinging and burning. The nasal bridge is the most frequently affected skin site and 83% of such cases occur due to the use of protective goggles but not with the hygiene mask. Excessive handwashing with detergents and disinfectants can affect the hydrolipid mantle of skin surfaces, cause irritation and also lead to the development of contact dermatitis [12].
Hands come in contact with the different surfaces throughout the day. Frequently touching the face through the hands would bring the germs and impurities to the face. Washing and sanitizing hands regularly with an alcohol-based sanitizer is the safest way to prevent the spread of the deadly coronavirus. As handwashing frequency has increased, there may be a concern about dry skin. The unnecessary use of alcohol-based sanitizers causes dryness and dehydration of skin. Handwashing with a soap can also cause dryness and dry skin also feels itchy and wrinkled [13].
In a study, Foo et al. investigated that 35.5% of the medical staff used N95 masks regularly, which caused facial dermatitis, acne and the pigmentation of cheeks, chin and nasal bridge. It was also reported that dermatitis with pruritic lesions mainly caused irritation, but allergic contact dermatitis occured because of the adhesives or other parts of the respiratory mask, like rubber straps and metal clips. In another study, Donovan et al., investigated the report on the N95 mask reactions during the time of the SARS epidemic in Toronto. The urticarial facial eruption was reported in 3 patients, 5 patients reported dermatitis and 2 patients were observed to have acute respiratory symptoms without skin lesions [14].
Yan et al., described the problems related to the skin caused by coronavirus. The health professionals working to prevent and control the spread of coronavirus are at the highest risk of having skin problems and damaged mucous membrane, which may lead to chronic and acute dermatitis, secondary infection and aggravation of underlying skin diseases. Latex gloves are mainly used to prevent coronavirus in the workplace, which causes maceration, softening, whitening and wrinkling of the skin [15].
CONCLUSION
The health professionals controlling the spread of coronavirus are prone to skin and mucous membrane problems. Insufficient and excessive protection will lead to adverse effects on the skin and mucous membrane barrier. The skin should be protected from the environment where viruses exist, for this, the required limited amount of soaps and sanitizers should be used. Patients with a skin disease should follow the proper medication to avoid contacting the virus. The symptoms of coronavirus also include skin problems, mainly on toes. It can cause rashes, irritation, blisters, acute and chronic dermatitis.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
Not applicable.
HUMAN AND ANIMAL RIGHTS
No animals/humans were used for studies that are the basis of this research.
CONSENT FOR PUBLICATION
Not applicable.
FUNDING
None.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
Declared none.


