All published articles of this journal are available on ScienceDirect.
Clear Cell Acanthoma of the Mammary Region: A Case Report
Abstract
Clear cell acanthoma, also known as Degos acanthoma, is a rare benign epithelial skin tumor. Generally, it appears as a solitary lesion on the lower legs, but in this case, it appeared on the right mammary area near the areola, which is an exceedingly rare and exciting finding. This lesion's clinical features revealed elevated dome-shaped plaque with surface lobulations and shiny pink color with a size of 9 mm. Dermoscopy was characteristic with blood vessels lined up in a strings pattern. Excision biopsy was done as a therapeutic measure. Histopathology showed a collection of glycogen-containing cells in the epidermis consistent with the diagnosis of clear cell acanthoma. Classical dermoscopy features and diagnostic histology were exemplary for a case report.
1. INTRODUCTION
Clear cell acanthoma is an uncommon, benign skin tumor of unknown etiology. Generally, it appears on the lower legs of middle-aged to elderly individuals with no gender predilection. Clear cell acanthoma is a well-defined, pink to reddish-brown plaque or nodule appearing on the skin with an average size of 5-10 mm. Commonly, the lesion is single but could be multiple also. Dermoscopy features are characteristic with blood vessels lined up in strings of pearls pattern. Though dermoscopy features were suggestive of the diagnosis, histopathology diagnosis was a must; hence excision biopsy was planned. Unfortunately, it was COVID-19 saga time; after necessary pre-procedure workup and negative COVID nasopharyngeal test, excision biopsy was done. Histopathology diagnosis was consistent with the clinical diagnosis and showed peculiar findings.
2. CASE REPORT
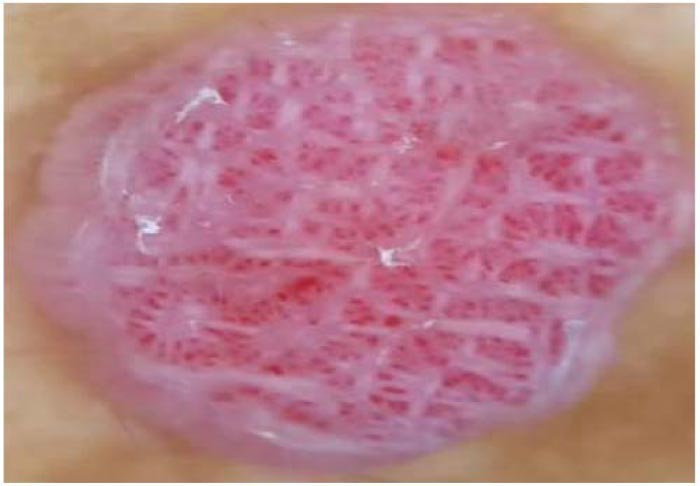
A 43-year-old male from Malaysia, residing in Dubai, came to the outpatient dermatology clinic at Saudi-German hospital Dubai with a chief complaint of a dome-shaped lesion in his right mammary region for two years with an interval increase in size in the last few weeks. He had mild pallor in the palpebral conjunctiva on general examination with a history of dengue hemorrhagic fever a few years back. The patient had no record of any metabolic disorder or medicine intake. The patient had nine mm-sized dome-shaped, lobulated, shiny pink-colored plaque in the right mammary region's skin on local dermatological examination. (Fig. 1)

2.1. Differential Diagnosis
The dermatological differential diagnosis for this morphology includes dermatofibroma, clear cell acanthoma, pyogenic granuloma, inflamed seborrheic keratosis, actinic keratosis, basal cell carcinoma, squamous cell carcinoma. Verruca vulgaris, psoriatic plaque, eccrine poroma, clear cell hidradenoma and melanoma [1].
2.2. Clinical Diagnosis and Dermoscopy
Dermoscopy picture was classical with glomerular and punctiform vessels with “pearl necklace” or “string of pearls’ distribution, features highly suggestive of clear cell acanthoma (Figs. 2 & 3). Vessels are organized in a reticular array. Although clinical and dermoscopy features are highly characteristic, excisional biopsy was a must.


2.3. Excision Biopsy
The patient was informed and made to understand the clinical as well as dermoscopy diagnosis. Verbal consent was obtained for photographs and future publishing. The patient was explained the need for lesion excision, and he accepted the same.
Unfortunately, the patient presented to OPD during the COVID-19 saga. According to the local health authority guidelines, a negative nasopharyngeal swab test was needed before proceeding to the excisional biopsy. The patient was also advised for routine preprocedural blood investigations.
Fortunately, the COVID-19 nasopharyngeal swab test was negative, and the patient consented to a biopsy.
Excisional biopsy was done under local anesthesia with a 3 mm negative surgical margin. The shape of the scar was crescentic with concavity towards the areola. The skin defect was closed with primary suturing after complete hemostasis was obtained. All necessary aseptic precautions were taken. Additional care was also taken, keeping in mind the ongoing COVID-19 pandemic. A biopsy sample was sent to the local hospital laboratory. The sample was examined after routine staining and block.
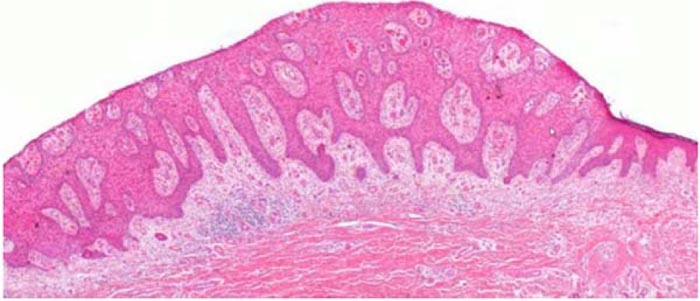
Excisional biopsy of the lesion with histopathological examination showed dilated blood vessels in the dermal papillae and proliferation of clear keratinocytes. Sharp demarcation between the pathological thickened epidermis and normal adjacent epidermis was noted.
The clear appearance of keratinocytes is due to vacuoles with glycogen as their contents on H & E staining (Figs. 4 & 5) confirmed by PAS staining. Histopathological diagnosis was confirmed as clear cell acanthoma without any atypical cells.
3. DISCUSSION
Clear cell acanthoma of the male mammary region is an exceedingly rare finding. Many case reports are available, quoting areolar and nipple involvement in females [2], but no case has been reported to date involving male patients' mammary region skin.
Usually, the lesion is solitary but can be multiple at times [3].
Though etiology is idiopathic, the simultaneous occurrence of clear cell acanthoma with few inflammatory skin diseases like psoriasis and atopic dermatitis suggests reactive phenomena secondary to chronic inflammation as etiopatho- genesis [3]. However, it would be worthwhile to keep regular follow-up of these patients to assess the new development of any inflammatory skin pathology.
Generally, clear cell acanthoma is an uncommon, asymptomatic benign epidermal tumor, which develops slowly over multiple years and remains stable for years [4]. Our patient also had the lesion for two years, but an interval increase in size within a few weeks, predominantly during “Lock-down” times of COVID-19, prompted him to consult and, in turn, remove. A sudden increase in size is also not a documented feature of clear cell acanthoma, which was a notable exception in this case. Malignant clear cell acanthoma has been described in the literature [5]. To date, only 3 cases have been reported of this malignant counterpart. Fortunately, the histopathologist was sure of the diagnosis without any other concomitant pathology or atypical malignant change. There are only a few reported cases of recurrence after excision in the literature [6, 7]. Kim CT et al. experienced that clear cell acanthoma had recurred at the excision site after two months [6]. As there are only a handful of recurrence cases without any definitive universal directives on the recurrent issue, this patient was asked to do a follow-up monthly for three months in the OPD. Till 3-month follow-up, no distortion or recurrence was seen in the nipple. The patient was explained to keep a close watch subsequently on the excision site on a 3-month follow-up visit and report any new lesion or change in scar morphology at the earliest in future.
CONCLUSION
In culmination, clear cell acanthoma can occur in the male mammary region without any predisposing inflammatory skin conditions. A malignant counterpart is a known rare opposite pole of this benign entity, which necessitates excision biopsy even though the dermoscopy findings are unique.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
Not applicable.
HUMAN AND ANIMAL RIGHTS
Not applicable.
CONSENT FOR PUBLICATION
Not applicable.
STANDARDS OF REPORTING
CARE guidelines have been followed.
FUNDING
None.
CONFLICT OF INTEREST
The author declares no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
Declared none.


