All published articles of this journal are available on ScienceDirect.
Carotid Intima-Media Thickness in Patients with Psoriasis
Abstract
Introduction:
Since the early 20th century, findings have demonstrated that psoriasis is frequently associated with atherosclerosis and cardiovascular diseases. The Carotid Intima-Media Thickness (CIMT) is a surrogate marker of atherosclerotic vascular disease.
Objective:
The aim of this study was to investigate the CIMT in patients with psoriasis and investigate its correlation with the clinical features.
Methods:
The present case-control study involved 70 patients with psoriasis who visited Ho Chi Minh City Hospital of Dermato-Venereology from September 2018 to April 2019 and 35 healthy subjects. Serum triglyceride, total cholesterol, high-density lipoprotein cholesterol, and low-density lipoprotein cholesterol levels were measured in both groups. Linear Doppler scanning was performed to evaluate the CIMT of the common, internal, and external carotid arteries and the presence of atherosclerotic plaques.
Results:
The mean CIMT value in psoriasis patients was significantly higher than that of controls [0.59 mm (0.53 - 0.71) vs. 0.54 mm (0.52 - 0.62), respectively, p = 0.036]. Multiple linear regression analysis revealed a significant correlation between the CIMT and age (p = 0.043) and CIMT and the Psoriasis Area and Severity Index (p < 0.0001). Moreover, the mean number of atherosclerotic plaques in psoriasis patients was significantly higher than that in controls [0.27 ± 0.68 vs. 0.03 ± 0.17, respectively, p = 0.035].
Conclusion:
Elderly patients with severe psoriasis should be evaluated carefully regarding CIMT and atherosclerotic plaques, as these signs are representative of increased cardiovascular risk.
1. INTRODUCTION
Psoriasis is a chronic inflammatory disease with the prevalence in the general population ranging from 0.51% to 11.43% in adults and 0% to 1.37% in children [1]. The progress of this disease is unpredictable, showing a persistent or recurrent course; no cure is currently available. Psoriasis may seriously affect patients’ quality of life and cause negative psychological issues, such as depression, emotional disorders, and suicidal thoughts. Moreover, many comorbidities are associated with psoriasis, including psoriatic arthritis, Crohn's disease, psychological or psychiatric disorders, and metabolic syndrome. Even though the cutaneous manifestations may ameliorate with routine treatments, the systemic involvements may progress chronically.
Psoriasis is a systemic inflammatory disorder that may be associated with atherosclerosis and cardiovascular comorbidities [2]. This theory was supported by the “psoriatic march,” in which the systemic inflammation causes insulin resistance, resulting in endothelial cell dysfunctions. Atherosclerosis increases the risk of fatal complications, such as myocardial infarction, ischemic stroke, and arterial embolism. Therefore, preclinical atherosclerotic screening is beneficial for the early perception of atherosclerosis progression. The rise in the Carotid Intima-Media Thickness (CIMT) is not only a surrogate marker of atherosclerotic damage, but also an independent predictor of myocardial infarction and stroke. Every 0.1 mm increase in the CIMT increases the risk of myocardial infarction by 10% to 15% and of stroke by 13% to 18% [3]. Atherosclerotic complications are typically present abruptly; however, the disease itself may have persisted asymptomatically for a long time. Currently, several methods are used for determining the carotid artery thickness, such as ultrasound, computed tomography, magnetic resonance angiography, and thoracic angiography. Among these, ultrasound is inexpensive, non-invasive, and extremely affordable. Furthermore, ultrasound machine is easily available without any health-related risks. Therefore, the CIMT measured using ultrasound has been readily used for the detection of atherosclerosis and its progression.
The CIMT cut-off value plays a vital role in the accurate assessment of cardiovascular risk in asymptomatic patients and early detection of coronary artery disease; this increases the efficacy of treatment and reduces mortality. Several studies have demonstrated an increase in the CIMT in patients with psoriasis and suggested the implementation of this measure to determine the cardiovascular risks in patients with psoriasis. Furthermore, Akdogan et al. recently reported that every 0.1 unit increase in the CIMT rose the risk of psoriasis 1.51-fold [4]. However, no study in Vietnam has investigated the association between CIMT and psoriasis. Therefore, this study aimed to investigate the CIMT and other corresponding factors, such as the clinical manifestations and risk factors for CIMT increase in patients with psoriasis. The findings of this study may contribute to the early detection of atherosclerotic plaques and cardiovascular events in psoriasis patients and provide physicians with a proper treatment plan.
2. MATERIALS AND METHODS
2.1. Study Design and Subjects
The present case-control study, involving 70 patients with psoriasis (group I) who visited the outpatient department of Ho Chi Minh City Hospital of Dermato-Venereology, Vietnam from Septemper 2018 to April 2019, was conducted after receiving institutional ethics clearance. A total of 35 age- and sex-matched healthy subjects were recruited as controls (group II). Patients aged > 18 years with any type of psoriasis, namely, psoriasis vulgaris, psoriatic arthritis, or erythrodermic psoriasis, were included. The diagnosis of psoriasis was based on clinical examination and histopathology if needed. Patients with comorbidities, such as diabetes, hypertension, connective tissue diseases (systemic lupus erythematosus, systemic sclerosis, and multiple myositis), Behcet’s disease, Sjogren’s syndrome, and rheumatoid arthritis and those with a previous history of cardiovascular or cerebrovascular disease were excluded. Participants were requested to avoid using estrogen hormone, cyclosporine, oral retinoids, antiplatelets, fibrates, statins, antihypertensive drugs, nitrates, or long-term corticosteroids, which may affect the CIMT measurement. The control group participants had no family history of psoriasis or other metabolic disorders.
2.2. Study Procedure and Measurements
In group I, both the history and clinical signs were recorded. Serum triglycerides, total cholesterol, High-Density Lipoprotein Cholesterol (HDL-C), and Low-Density Lipoprotein Cholesterol (LDL-C) levels were measured in both groups. Doppler ultrasound using a linear Doppler scan 11L-D (4.5-12 MHz) (Vivid S70 N, General Electric Company, Norway) was performed by a radiology expert to identify the CIMT of the Common Carotid Artery (CCA), Internal Carotid Artery (ICA), and External Carotid Artery (ECA), and the presence of atherosclerotic plaques. The CIMT was determined in the following positions on both sides: 1) in the CCA, 1 cm inferior to the carotid sinus, 2) the proximal third of the ICA and 3) the proximal third of the ECA in both groups. According to the European Society of Cardiology/European Society of Hypertension (ESC/ESH) 2003 guidelines, CIMT < 0.9 mm is classified as normal, and CIMT between 0.9 and 1.5 mm is classified as an increase in the intima-media thickness [5]. The presence of an atherosclerotic plaque was defined as CIMT > 50% of the thickness of the nearby artery and protruding > 0.5 mm into the inner layer of the artery or CIMT ≥ 1.5 mm.
2.3. Statistical Analysis
Data are presented as mean and Standard Deviation (SD), median and range, or prevalence when appropriate. The Mann-Whitney U test or a t-test was used to compare the mean values between the two groups. Spearman’s rank correlation coefficient was used to investigate the correlation between the parameters. A p-value < 0.05 was considered statistically significant. Multivariate regression analysis was used to determine the correlation between multiple variables. Statistical analyses were operated using Stata version 14 (StataCorp. 2015 Stata Statistical Software: Release 14 College Station, TX: StataCorp LP).
2.4. Ethical Considerations
This study was approved by the Research Ethics Committee of Ho Chi Minh City Hospital of Dermato-Venereology, Vietnam (Ethical approval number: 390/QĐ-BVDL on 17th August 2018). All of the volunteers were informed, and they signed a consent form related to the study; they were told that they could withdraw at any time without any effects on their treatment at the hospital. All patients’ data were kept confidential and only used for research purposes.
3. RESULTS
3.1. Clinical Manifestations of the Study Subjects
This study comprised 70 patients with psoriasis and 35 healthy age- and sex-matched controls. No significant differences were observed in the age, sex, smoking habit, alcohol use, and Body Mass Index (BMI) between the two groups. The difference between the levels of triglycerides, cholesterol, HDL-C, and LDL-C among psoriasis patients and controls was not statistically significant (Table 1).
| Characteristics | Psoriasis Patients (N = 70) | Healthy Group (N = 35) | P-value |
| Age (median, IQR) | 41 (30.54) | 44 (31.54) | - |
| Highest | 72 | 63 | 0.989(1) |
| Lowest | 18 | 22 | - |
| Age at onset (mean ± sd) | 31.7 ± 14.7 | - | - |
| Sex (n, %) | - | - | - |
| Female | 21 (30%) | 10 (29%) | 0.880(2) |
| Male | 49 (70%) | 25 (71%) | - |
| Smoking (n, %) | - | - | - |
| Yes | 45 (64%) | 26 (74%) | 0.302(2) |
| No | 25 (36%) | 9 (26%) | - |
| Alcohol (n, %) | - | - | - |
| Never | 35 (50%) | 23 (66%) | 0.281(2) |
| Once a month | 21 (30%) | 10 (28%) | - |
| 2-4 times/month | 7 (10%) | 2 (6%) | - |
| 2-3 times/week | 5 (7%) | 0 | - |
| > 3 times/week | 2 (3%) | 0 | - |
| BMI (n, %) | - | - | - |
| Underweight | 7 (10%) | 0 | 0.266(2) |
| Normal weight | 56 (80%) | 31 (88%) | - |
| Pre-obesity | 6 (9%) | 3 (9%) | - |
| Obesity | 1 (1%) | 1 (3%) | - |
| PASI Score | |||
| PASI (mean ± sd) 16.73 ± 9.86 - | |||
| Blood Lipid Levels | |||
| Triglyceride (median; IQR) | 1.6 (1; 2.2) | 1.4 (0.8; 2) | 0.302(1) |
| Cholesterol (mmol/L) | 4.75 ±1.08 | 5.06 ± 1.15 | 0.148(3) |
| HDL-C (mmol/L) | 1.34 ± 0.39 | 1.18 ± 0.49 | 0.526(3) |
| LDL-C (mmol/L) | 2.55 ± 0.89 | 2.85 ± 0.88 | 0.159(3) |
(1) Mann-Whitney U test, (2) Chi-square test, (3) T-test, IQR: interquartile range
The mean disease duration was 10.4 ± 7.5 years (range, 01 - 30 years), whereas the mean age of onset was 31.7 ± 14.7 years; 57% of the patients were afflicted with the disease before the age of 30. In this study, plaque psoriasis was the most dominant form with 49 cases (70%), whereas psoriatic arthritis and erythrodermic psoriasis were observed in 14 (20%) and 7 (10%) patients, respectively. The Psoriasis Area and Severity Index (PASI) score was also evaluated in patients with plaque psoriasis and psoriatic arthritis (n = 63). The mean PASI score for these types was 16.73 ± 9.86 (range: 1.2 - 45.7). The difference in the PASI scores between the two types was statistically insignificant.
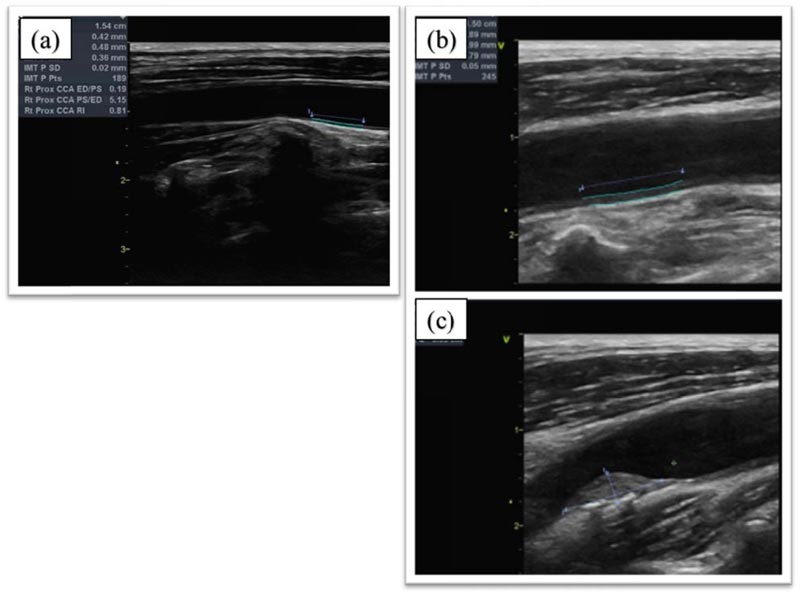
3.2. Ultrasonographic Characteristics
The magnitude of CIMT change in the CCA, ICA, and ECA was measured both in patients and in healthy volunteers. The CIMT value of the CCA in psoriatic patients [0.59 mm (0.53 - 0.71)] was statistically higher than that of controls [0.54 mm (0.52 - 0.62), p = 0.036]. Similarly, the ECA was thicker in psoriasis patients than in controls [0.62 mm (0.55 - 0.70 vs. 0.56 mm (0.50-0.67), respectively, p = 0.046]. The diameter of the atherosclerotic plaques in psoriasis patients was 0.27 ± 0.68 mm and was statistically greater than that of controls (0.03 ± 0.17 mm) (p = 0.035) (Fig. 1a, b and c). However, no statistically significant difference was observed in the ICA diameter between the two groups [0.64 mm (0.56 - 0.72) vs. 0.61 mm (0.53 - 0.66), respectively, p = 0.134] (Table 2).
| Characteristics | Psoriasis Group | Normal Group | p-value(*) |
| Median (25%, 75%) | Median (25%, 75%) | ||
| CCA (mm) | 0.59 (0.53, 0.71) | 0.54 (0.52, 0.62) | 0.036 |
| Max | 1.2 | 0.86 | - |
| Min | 0.42 | 0.44 | - |
| ICA (mm) | 0.64 (0.56, 0.72) | 0.61 (0.53, 0.66) | 0.134 |
| Max | 1.3 | 0.85 | - |
| Min | 0.44 | 0.45 | - |
| ECA (mm) | 0.62 (0.55, 0.7) | 0.56 (0.50. 0.67) | 0.046 |
| Max | 1.3 | 0.75 | - |
| Min | 0.44 | 0.46 | - |
| Atherosclerosis plaque | - | - | 0.035 |
| Max | 0.27 ± 0.68 | 0.03 ± 0.17 | - |
| Min | 3 | 1 | - |
| - | 0 | 0 | - |
(*) Mann-Whitney U test
3.3. Association between the CIMT and Clinical Features
There was no relationship between the CIMT and sex, BMI, and alcohol usage. A subgroup analysis demonstrated a statistically higher CIMT value in smokers than in non-smokers [0.68 mm (0.60 - 0.72) vs. 0.56 mm (0.52 - 0.68), respectively, p = 0.009] as well as in patients with late disease onset than in patients with early-onset [0.69 mm (0.58 - 0.8) vs. 0.55 mm (0.52 - 0.64), respectively, p = 0.002] (Table 3).
| Characteristics | Total | CIMT (mm) | ||
| Mean | SD | P-value | ||
| Sex | - | - | - | - |
| Male | 49 | 0.62 (0.52; 0.74) | 0.61 - 0.71 | 0.149(1) |
| Female | 21 | 0.56 (0.54; 0.6) | 0.55 - 0.61 | - |
| BMI | - | - | - | - |
| Underweight | 7 | 0.58 (0.56; 0.74) | 0.45 - 0.90 | - |
| Normal weight | 56 | 0.57 (0.52; 0.7) | 0.59 - 0.77 | 0.79(2) |
| Pre-obesity | 6 | 0.65 (0.58; 0.74) | 0.55 - 0.74 | - |
| Obesity | 1 | 0.64 (0.64; 0.64) | - | - |
| Smoking | - | - | - | - |
| Yes | 25 | 0.68 (0.6; 0.72) | 0.62 - 0.74 | 0.009(1) |
| No | 45 | 0.56 (0.52; 0.68) | 0.57 - 0.66 | - |
| Alcohol | - | - | - | - |
| Never | 35 | 0.56 (0.52; 0.7) | 0.58 - 0.69 | 0.454(2) |
| Once a month | 21 | 0.64 (0.56; 0.74) | 0.60 - 0.74 | - |
| 2 - 4 times/month | 7 | 0.62 (0.52; 0.68) | 0.54 - 0.69 | - |
| 2 - 3 times/week | 5 | 0.58 (0.55; 0.61) | 0.50 - 0.69 | - |
| 3 times/week | 2 | 0.51(0.46; 0.56) | 0.13 - 1.15 | - |
| Disease onset | - | - | - | 0.0002(1) |
| Early | 40 | 0.55 (0.52 - 0.64) | 0.55 - 0.61 | |
| Late | 30 | 0.69 (0.58 - 0.80) | 0.64 - 0.78 | |
In univariate analysis, CIMT exhibited a positive relationship with age (r = 0.63, p < 0.001) and the PASI score (r = 0.38, p=0.002). However, no correlations were observed between CIMT and disease duration or the triglyceride, cholesterol, HDL-C, and LDL-C levels (p > 0.05). In multivariate regression analysis, the relationships between the CIMT and age and CIMT and PASI were statistically significant (p = 0.045 and p = 0.000, respectively) (Table 4).
| Value | B | β | t | P-value |
| Constant value | 0.33 | - | - | - |
| Age | - | 0.003 | 2.05 | 0.045 |
| Female | - | 0.034 | 1.02 | 0.313 |
| Male | - | 0.6 | 1.03 | 0.308 |
| Disease onset | - | 0.002 | 1.57 | 0.123 |
| PASI | - | 0.006 | 3.73 | 0 |
4. DISCUSSION
We found that the CIMT value in the psoriasis group was higher than that in controls (p < 0.05), and this difference was statistically significant. This result was concurrent with that of a study by Balci et al. in which the CIMT values at the left, right, and mean positions were higher in the psoriasis group than in the healthy group (0.607 ± 0.44 mm vs. 0.532 ± 0.01 mm, 0.611 ± 0.157 mm vs. 0.521 ± 0.17 mm, and 0.609 ± 0.16 mm vs. 0.526 ± 0.14 mm, respectively, p < 0.01) [6]. Similar findings (statistically higher CIMT values in the psoriasis group than in the control group) were observed in studies by Troitzsch et al. [7], Enany et al. and Yiu et al. (0.73 ± 0.11 mm vs. 0.67 ± 0.08 mm, respectively, p<0.01), and Antonucci et al. (Italy) (1.465 ± 0.53 mm vs. 0.89 ± 0.27, respectively, p < 0.001) [8-10]. Di Minno et al. conducted a literature review including 12 studies which revealed that the CIMT value was statistically higher in 759 patients with psoriatic arthritis than in 937 healthy controls (p < 0.001) [11]. A similar result was observed in the study by Dünya et al. in 2015, which compared the CIMT in 42 patients with psoriatic arthritis and 30 healthy individuals (0.76 ± 0.15 mm vs. 0.57 ± 0.12 mm, respectively, p < 0.001) [12]. A Malaysian study by Mazlan et al. involving 63 patients with psoriatic arthritis concluded that 16% of the patients had a mean CIMT of 0.725 ± 0.260 mm [13]. The difference between the two groups with respect to the corresponding CIMT factors such as age (p = 0.005), waist circumference (p = 0.001), hypertension (p = 0.007), diabetes (p = 0.002), and metabolic syndrome (p = 0.001) was also statistically significant [14]. In contrast, Kim et al. evaluated the CIMT and stiffness of the artery in 54 patients and 60 age- and sex-matched healthy controls and reported that although the CIMT value in the psoriasis group was higher than that in controls, this difference was not statistically significant (p = 0.076). However, this study found that only the stiffness of the artery was statistically correlated to age, systolic pressure, and disease severity [15]. According to a cross-sectional study enrolling 62 patients with plaque-type psoriasis and 31 age- and sex-matched controls, CIMT was considered an independent risk factor for psoriasis [4]. In summary, most studies showed that the CIMT value was higher in psoriatic patients compared with controls.
Atherosclerosis, a critical process in cardiovascular disease, is inflammatory in origin. Psoriasis is a systemic inflammatory disease that is presented with an increase in the conventional inflammatory cytokines and adipokines, such as resistin and leptin. Adipokines in the serum of psoriasis patients are similar to those seen in prediabetic patients and are strong predictors of an insulin-resistant condition. In addition to insulin resistance, excessive adipokines may result in atherosclerosis through immune regulatory mechanisms, such as improved endothelial cell linkage. At the level of the endothelial cells, insulin resistance causes endothelial cell dysfunction, consequently making the arteries stiffer. This cascade results in an increase in the CIMT and calcification of the carotid artery, thus increasing the risk of severe cardiovascular comorbidities, such as myocardial infarction and stroke [16]. Moreover, proinflammatory cytokines, such as Tumor Necrosis Factor-alpha (TNF-α) and interferon found in psoriasis, play a vital role in endothelial dysfunction and atherosclerotic plaque formation [17].
Age, sex, smoking, alcohol use, BMI, and obesity are known to increase the CIMT. However, we observed that only a history of smoking showed a significant association; smokers exhibited a significantly higher CIMT value (0.68 mm) than non-smokers (0.56 mm, p = 0.009). In smokers, either the inflammatory process or reduced internal fibrinolysis was suggested to correlate with atherosclerotic pathology [18]. We found that CIMT had a positive correlation with age (r = 0.63, p < 0.001) and the PASI (r = 0.38, p = 0.002). This correlation between the CIMT and PASI was not only due to the chronic inflammation but was also related to artery growth factors, such as the Vascular Endothelial Growth Factor (VEGF). VEGFs are produced by the keratinocytes in psoriatic lesions and are strongly related to the disease severity and an increase in the IMT [7]. Several studies have exhibited a decrease in the CIMT after psoriasis treatment. A decrease in the CIMT (p = 0.010) was observed in a 2-year follow-up study by Tam et al. in patients with psoriatic arthritis who were treated with monoclonal antibodies against TNF-α [19]. A similar result was obtained in a study by Jókai et al. (p = 0.0002) [20]. In 2018, Martinez-Lopez et al. demonstrated that CIMT tended to decrease with biological treatments, particularly with anti-IL-12/23 agents and methotrexate in patients suffering from moderate and severe psoriasis [21]. However, additional larger studies are needed to fully confirm the association between psoriasis treatment and CIMT decrease.
The number of atherosclerotic plaques in psoriasis group patients was statistically higher than that in healthy controls, which was in accordance with the results of the study by Di Minno et al. [11]. Inflammation, triggered by the autoimmune response to plaque antigens, such as oxygenated LDL and heat shock protein, is thought to induce the formation and development of atherosclerotic plaques. The promotion of self-activating T helper type 1 (Th1) cells and a decrease in moderator T cells induces the release of proinflammatory cytokines, such as TNFα, interleukin (IL)-1β, and IL-6; these are the common pathways among the genetic predisposition, leading to atherosclerosis, arthritis, and psoriasis [22]. The presence of atherosclerotic plaques is considered a more credible prognosticator of cardiovascular accidents than the CIMT [23].
This was a case-control study that allowed us to evaluate the significant difference between the CIMT value of psoriatic patients and healthy volunteers. This result supports the measurement of CIMT through ultrasound in clinical practice to help identify patients at high cardiovascular risks. However, our research had some limitations. First of all, our sample size was still modest. Secondly, we did not follow up with the patients to determine the effects of treatment on the CIMT. Thus, more comprehensive researches are warranted with a larger sample size to identify the CIMT cut-off value in psoriasis patients. Furthermore, the correlations between the change of CIMT value and clinical manifestations in psoriasis patients before and after systemic treatments remain to be elucidated in the near future.
CONCLUSION
The CIMT value in the psoriatic group was higher than that in healthy controls. Although no correlation was found between the CIMT and serum lipid levels, a positive relationship between the CIMT and age, as well as PASI (p < 0.0001), was observed. The number of atherosclerotic plaques in the psoriasis group was significantly higher than that in the control group. From these results, we concluded that ultrasound is a simple, non-invasive technique for evaluating the CIMT and the number of atherosclerosis plaques. This will assist in the diagnosis of preclinical atherosclerosis and will screen individuals at high risk of cardiovascular events. Elderly patients with severe psoriasis should be evaluated carefully with regard to the CIMT, and atherosclerotic plaques as these signs are representative of increased cardiovascular events.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
This study was approved by the Research Ethics Committee of Ho Chi Minh City Hospital of Dermato-Venereology, Vietnam (Ethical approval number: 390/QĐ-BVDL on 17th August 2018).
HUMAN AND ANIMAL RIGHTS
No animals were used in this research. All human research procedures followed were in accordance with the ethical standards of the committee responsible for human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2013.
CONSENT FOR PUBLICATION
All of the volunteers were informed, and they signed a consent form related to the study.
AVAILABILITY OF DATA AND MATERIALS
Not applicable.
FUNDING
None.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
Declared none.


