All published articles of this journal are available on ScienceDirect.
Insights into Alopecia Areata: A Systematic Review of Prevalence, Pathogenesis, and Psychological Consequences
Abstract
Background
Alopecia areata is an autoimmune condition distinguished by visual non-scarring hair loss in different head and face regions. The condition affects every age group and is prevalent in all types. Alopecia areata is a disorder that arises from a malfunction of the immune prerogative of the hair follicle, which can be managed with new treatments and remission.
Objective
This study aimed to determine the psychological impacts of Alopecia, the frequency of the condition, and its impact on quality of life.
Methods
Data from relevant studies conducted between 2018 and 2023 were collected using the PRISMA criteria and the SPIDER framework. For this review, 15 studies were selected using specific keywords, such as Alopecia Areata, Alopecia Prevalence, Alopecia areata management, and Alopecia areata treatment on 8 search engines, such as PubMed, Scopus, Google Scholar and more. The papers were selected through inclusion and exclusion criteria. Psychological factors, such as mental health, anxiety, stress and depression, were found to play a significant role in this autoimmune condition.
Results
The updated approach in this study analyzes the prevalence of Alopecia areata,its impacts on daily life, and underlying mechanisms. It emphasizes the psychological burdens and advocates for awareness, education, and support for affected individuals.
Conclusion
This systematic review advances the understanding of the prevalence of Alopecia areata and its psychological effects, with potential implications for healthcare practices and policy decisions.
1. INTRODUCTION
Alopecia areata is an autoimmune disorder that causes non-scarring hair loss or fall. It starts with a disruption in the hair follicle, making it weak, so the hair falls out [1]. Alopecia areata may incite in one or all parts of the head in patches, also called patchy baldness [2]. Alopecia areata also affects facial hairs and can develop anywhere on the scalp, beard, eyebrow, eyelashes, ear, etc [3]. Alopecia areata (AA) is the loss of hair places ranging in size from roughly 1 cm to large areas on the scalp [4]. Pregnant women may experience little patches of hair loss as well [5]. People with AA may experience spontaneous remission but may also experience repeated attacks [6]. The type, color, and texture of regrown hair may not always resemble the original hair [6]. There are times when AA reacts to the medication, although its effectiveness is debatable [7].
1.1. Types and Prevalence of AA
The types of Alopecia can vary subsequently; Alopecia Universalis (AU) depicts the complete loss of hair on the head and body, as opposed to alopecia totalis (AT), which only affects the head. Then, there is Alopecia ophiasis (AO), a rare subtype of alopecia areata that starts to occur from the back and sides of the head [8]. The likelihood of the patient experiencing a significant improvement in hair development is much lower for AU and AT of Alopecia than for AA [8]. About 7–30% of all alopecia areata are estimated to be caused by Alopecia totalis and universalis [9]. About 60% of Alopecia areata patients observe their first bald patch before the age of 30, and the average lifetime risk of the condition is believed to be between 1.7 and 2.1%. Around 20% of instances involve minors [10].
1.2. Mechanism of Action
The exact mechanism of action that causes alopecia areata is not yet known; it is thought to be an autoimmune illness. In alopecia areata sufferers, the immune system unintentionally targets the hair-producing hair follicles of the skin. This assault causes the hair follicles to inflame and die, which causes hair to fall out [11]. The hair follicle is essential to the skin, with immunological privileges and the ability to evade an immune cell attack. The inhibition of immune cell activation in hair follicles results from decreased Major histocompatibility complex (MHC class I and 2) microglobulin exhibition in the hair bulb [12]. According to histological analysis, patients with alopecia areata had inflammatory cell invades in the bulbar parts of their hair follicles [12]. The hair network epithelium goes through a crucial phase called hair shaft cortical differentiation, influenced by immune cell responses at the time [13]. Following immune cell responses to hair follicles, MHC class I and class II exhibition in the pre-cortical hair shaft is increased, which causes vacuolar degeneration and impairs the strength of the hair shaft. It is believed that decreased exhibition of MHC class I and II and macrophage migration inhibitory factor (MIF) inhibits T cell and CD56+ NKG2D+ NK cell activity [13-15].
Further, Alopecia areata is hypothesised to be stimulated by several genetic, environmental, and immune system variables [16]. According to some studies, certain genes may predispose people to the illness. At the same time, other research contends that environmental stimuli, including viral infections or stress, may also contribute to the immunological response [1]. When the immune system invades the hair follicles, T-cells, immune cells that are crucial in the fight against infections and disorders, are created. These T cells target the Alopecia areata hair follicles, inflaming and destroying them. This results in round or oval areas of hair loss [17]. In addition to the role of the immune system, other factors may contribute to hair loss in alopecia areata, such as changes in hair follicle structure, hormonal imbalances, and nutritional deficiencies [18]. However, extensive research is required to understand the underlying mechanisms of alopecia areata fully.
1.3. Contributing Factors
Various reasons that may contribute to the development of alopecia areata include:
- Since alopecia areata frequently runs in families, it has a genetic basis. Studies have found numerous genes to potentially impact the illness (Lepe & Zito, 2022). An autoimmune illness like alopecia areata occurs when the immune system of the body unintentionally destroys its cells. Alopecia areata may be more common in those with other autoimmune diseases, such as type 1 diabetes or rheumatoid arthritis [19].
- Some environmental triggers, such as viral infections, stressful life events, and physical injury, may trigger the genesis of alopecia areata in susceptible individuals [16].
- Hormonal changes, such as those that occur during pregnancy or menopause, may contribute to the development of alopecia areata [20].
- Deficiencies in certain nutrients, such as iron, vitamin D, or zinc, may contribute to hair loss and may be associated with alopecia areata [21].
- Certain medications, such as those used to treat cancer or autoimmune disorders, may cause hair loss as a complication [22].
- Psychological factors, such as anxiety or depression, may help develop alopecia areata, as stress can impact the immune system and may trigger the genesis of the condition [23].
1.4. Impact on Daily Life
One study found that individuals with alopecia areata had lower quality-of-life scores than those without the condition. The impact on quality of life was greater for those with more severe hair loss [24]. Hair is often considered an important aspect of the appearance and identity of a person, and hair loss can be a visible sign of illness or disability. This can lead to stigma and discrimination, further exacerbating the psychological impact of alopecia areata. Children with alopecia areata may also experience difficulties in social settings and may be at risk of bullying and teasing from peers [25]. Parents and caregivers of children with alopecia areata may also experience psychological distress and anxiety related to the condition of their child [25]. According to a recent study, at least 23% of patients encountered a psychological problem or trauma before developing alopecia areata [26, 27].
This study aims to determine the global prevalence and psychological impacts of alopecia areata on quality of life and to investigate various factors influencing the disorder by reviewing several relevant studies. This review delves into the global prevalence and psychological effects of Alopecia Areata, with a global prevalence of around 2%. The condition predominantly affects children and young adults, causing symptoms, such as social isolation, depression, and anxiety. Importantly, this study addresses the research question: 'What is the current state of knowledge regarding the global prevalence of Alopecia areata and its psychological effects, based on recent studies published between 2018 and 2023?' Psychological factors, including mental health, anxiety, stress, and depression, emerge as significant contributors to the development of the disease. The review emphasizes the dire need for comprehensive treatment options that include both medical and psychological therapy in light of these findings. Additionally, it promotes awareness to identify the root causes of the disease and develop effective solutions. The study highlights the value of raising awareness, providing education, and creating support systems for people who are dealing with alopecia areata.
2. METHODOLOGY
In order to determine the global prevalence and effects of Alopecia areata on psychology, several studies were included. The systematic review was done utilizing the PRISMA guidelines and checklist [28]. The author selected, evaluated and retrieved data from the analysis. The papers that would be incorporated in our systematic reviews were selected using the SPIDER framework, as indicated in Table 1.
2.1. Search Strategy
Different keywords were used on different databases. Abstracts and titles were matched to see the duplication. Duplicate articles were eliminated after reviewing and checking the availability. PICO was employed as a search strategy tool in multiple databases, as shown in Tables 2 and 3.
2.2. Literature Selection
Databases like Scopus, PubMed, Google Scholar, Elsevier, Web of Science, Sage, Cochrane, and Medline were used to compile the data of this systematic study. To organize the material, the filtering options of the available search channels were used. Articles published between January 2018 and January 2023 were analyzed to determine the differences in the prevalence and occurrence of Alopecia Areata, as well as its psychological effects. The review emphasizes various related topics, including Alopecia areata, Alopecia areata prevalence, occurrence, impacts on daily life, factors influencing the disorder and the mechanism of the disorder. Several other terms were incorporated, including longitudinal, prospective, retrospective, case study, cohort, reviews, and follow-up. The terms chosen are presented in Table 3.
| Sample | Adults, Young Adults, Elderly |
|---|---|
| Phenomenon of Interest | Impacts and effects of Alopecia areata |
| Design | Review of already published articles using Search engines. |
| Evaluation | Alopecia areata |
| Research Type | Case report, controlled study, cohort, prospectives, retrospective, observational, reviews. Retrospective, longitudinal, and qualitative analysis. |
| No. | Search Strategy (PICO- Population Intervention Comparison Outcomes) |
|---|---|
| 1 | Alopecia, Alopecia Areata OR, Alopecia Prevalence Or Alopecia patients Or Alopecia areata management OR Alopecia areata update. |
| 2 | Alopecia areata treatment OR Alopecia Intervention [Abstract & Keywords] Prevalence globally [Abstract & Keywords] OR Factors influencing Alopecia [ Abstract & Keywords] OR Psychological Impacts Alopecia. |
| 3 | Quality of Life OR Stress in Alopecia OR Epidemiology OR Genetics OR Alopecia areata diagnosis OR Autoimmune disorder OR Alopecia areata treatment options OR Psychological stressful outcomes of the disorder. |
| Years | Search Engines | Keywords |
|---|---|---|
| 2018-2023 |
 Google Scholar Google Scholar Scopus Scopus Web of Science Web of Science MEDLINE MEDLINE PubMed PubMed Elsevier Elsevier Cochrane Cochrane Sage Sage |
 Alopecia Areata Alopecia Areata Alopecia Areata global prevalence Alopecia Areata global prevalence Quality of Life OR Stress in Alopecia Areata Quality of Life OR Stress in Alopecia Areata Alopecia areata diagnosis Alopecia areata diagnosis Factors influencing Alopecia Factors influencing Alopecia Alopecia areata treatment and management Alopecia areata treatment and management |
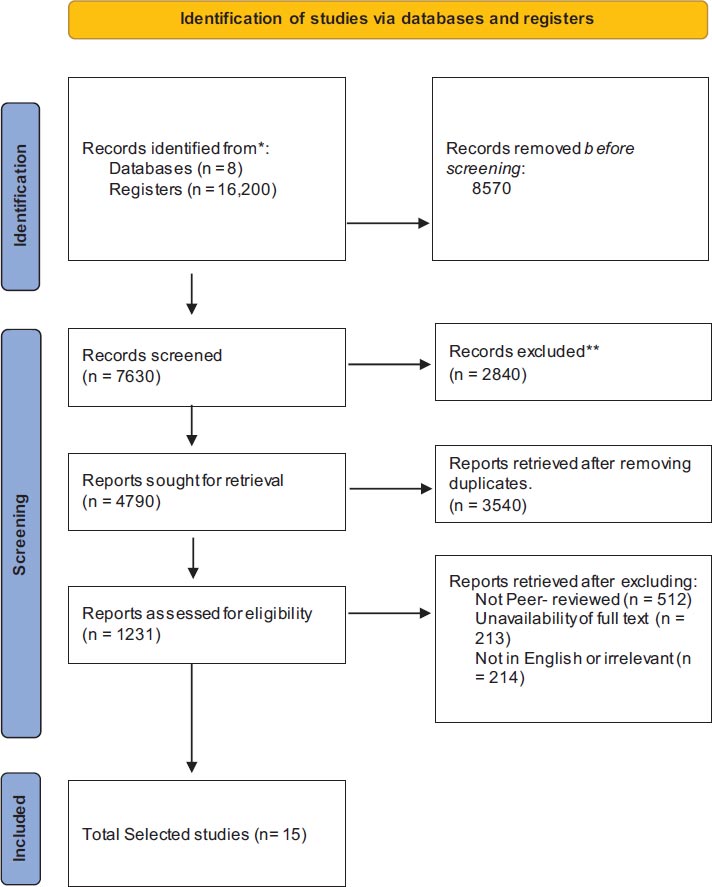
The latest scientific articles on alopecia areata were broadly welcoming. The best available research was gathered by looking at publications with a high impact. The articles had to meet the following criteria (Fig. 1).
2.3. Research Design
2.3.1. Inclusion Criteria
The goal was to include and incorporate high-quality, pertinent studies. Studies that directly related to the subject of this review were included. A key stage in this evaluation is the selection of the studies to be investigated, as they require a thorough analysis and screening of all the search results. Based on the points mentioned previously, the inclusion criteria are as follows:
- Directly Relevant studies were included.
- Studies based on the prevalence and psychological impacts of alopecia areata were included.
- Studies in the selected search range of 2018-2023 were included.
- Peer-reviewed and published studies were included.
- Studies written in English were selected to provide a better understanding medium to the researchers and the readers.
2.3.2. Exclusion Criteria
Studies were excluded or deducted based on criteria that were insufficient for the subject of this study and interfered with the writing process. By excluding publications that were not related to the research, exclusion criteria narrowed down the evaluation. The following criteria determined exclusions.
- Studies that were not directly related to the subject, studies related to alopecia areata other classes.
- Studies older than the selected range were also excluded
- Studies that were not full text and no experimentation or case study were reported.
- Studies based on a language other than English.
2.4. Study Selection
The study aimed to include relevant, latest or current, updated studies on Alopecia areata. A cumulative amount of 16,200 documents were collected from the included databases: PubMed, Elsevier, Google Scholar, Scopus, Sage, Medline, Web of Science and Cochrane, upon using the database filter of year. The studies were retrieved from the year 2018-2023. The study focuses on the latest developments and trends in the field of Alopecia areata, focusing on the last five years. This approach acknowledges the evolving advancements of research and ensures the inclusion of the latest findings. The selected timeframe aligns with the objective of the study, providing insights into the current prevalence and psychological impacts of Alopecia areata.
Additionally, the study maintains methodological consistency by focusing on a specific timeframe, facilitating a more cohesive analysis of selected studies. The studies include observational, prospective, retrospective, cross-sectional, cohort, original and reviews. After using the specific keywords to obtain the most relevant data, 7,630 studies were retrieved; these studies were further filtered by using the keywords Prevalence and Psychological Impacts of Alopecia Areata, and the data retrieved were 4,790. The search results were further reduced to 3,450 by removing duplicates. These search results underwent the inclusion and exclusion criteria of the study. After examining the abstract and title, irrelevant studies were discarded, and the data retrieved were 1,231. Out of these 1,231, some studies were removed due to not being peer-reviewed yet, and the number of studies came down to 512.
In contrast, some studies were removed for the unavailability of full text and due to language barrier, as the criteria for studies to be included was to be in the English language. The data came down to 85. Out of these 85 studies, 15 of the most relevant, latest and contributing studies were selected to understand better the disorder regarding its global prevalence and repercussions on quality of life. A Prisma flowchart is placed below, which summarises the study selection process.
2.5. Quality Assessment of Selected Studies
The review comprises a thorough quality assessment process for selected papers. This includes assessing the methodological accuracy, study design, and data reliability in each study.
Evaluation of the research design: Well-designed studies, including controlled trials, prospective and retrospective cohort studies, and case-control studies, were preferred.
Sample Size: To guarantee that the study can produce significant results, the sample size and statistical power were taken into account.
Peer Review: This included works that have undergone peer review in order to uphold a standard of scientific rigor.
Methodological soundness: The process of evaluating the overall quality of each study by closely examining the procedures used in data collection, analysis, and interpretation.
3. RESULTS
This study examined the impact of Alopecia areata on quality of life. About 16,200 papers were obtained from databases and retrieved from 2018-2023. After using keywords to obtain relevant data, 7,630 studies were retrieved and further filtered using prevalence and psychological impacts. The search results were further reduced to 3,450 by removing duplicates. Of these 85 studies, 15 of the most relevant, latest and contributing studies were selected.
This review of 15 selected studies hypothesized that depending on the population being investigated and the diagnostic standards being applied, the prevalence of alopecia areata might vary significantly. The disorder can affect people of different ages, genders, and races and strike at any point in the life of a person. Although it can happen at any age, it is most frequently diagnosed in children and young people. Alopecia areata is not considered a rare disease. Nonetheless, it can significantly influence the quality of life of an individual and may need regular medical attention and treatments. The studies presented a comprehensive analysis of AA, focusing on its impact on quality of life, long-term course assessment, psychosocial burden, associations with mental health disorders, patient satisfaction, psychosexual effects, and childhood AA characteristics.
- AA prevalence varies significantly across populations, with higher rates observed in certain regions like India.
- Childhood AA is prevalent, with scalp involvement being the most common type.
- Specific hair loss patterns like ophiasis can be indicative of severe AA.
- Atopic disorders may be associated with childhood AA.
- Gender differences exist in terms of psychological impacts, with females experiencing more negative effects.
- AA is strongly linked to both anxiety and depression, with adults and those with severe hair loss being at higher risk.
- Mental health status significantly impacts patient satisfaction with healthcare in AA cases.
- Early psychological intervention can improve overall well-being and healthcare satisfaction for AA patients.
- Androgenetic alopecia (AGA) progression is associated with increased vulnerability to psychosexual disorders, highlighting the need for early support.
- Children with AA may develop PTSD following traumatic events, requiring specialised care.
- Psychiatric evaluation and interventions are crucial in addressing mental health challenges associated with AA.
- The presence of AA alone significantly increases the risk of anxiety and depression.
- AA patients experience significant psychosocial burden and impaired QoL.
- The prevalence of severe AA, duration of the initial episode, and rate of relapses decrease with older age at onset.
- AA is significantly associated with anxiety and depression.
- Parents of pediatric AA patients experience impaired QoL, which is linked with the intensity of the disease and the age of the afflicted child.
- The prevalence of AA in Saudi Arabia is 2.3%, with a higher prevalence in pediatric cases.
- Comorbid conditions, including hypothyroidism, diabetes mellitus, and atopic diseases, are common in AA patients.
Further research is needed to investigate the complicated link between AA and mental health, particularly in terms of age and disease severity.
4. DISCUSSION
AA is a disorder when the immune system attacks hair follicles. The condition can affect hair on the scalp and other body parts, like eyebrows, eyelashes, and beard [29]. The exact cause of alopecia areata is not completely understood; however, it is believed to be an autoimmune disorder [30]. Alopecia areata can occur at any age and affects males and females equally. The condition can be unpredictable, with hair loss and regrowth cycles occurring intermittently. Alopecia areata has no known cause or therapy, although several ways exist to manage the illness and encourage hair growth [30].
This study is focused on evaluating the prevalence and psychological impacts of Alopecia areata, according to one of the selected cross-sectional studies held in Nepal over one year. The study included all participants with a new rise of AA. A thorough history was gathered, an examination performed, and a dermatologist consultant established the clinical diagnosis. A biopsy was carried out in cases of diagnostic uncertainty. The study results concluded that the incidence of depression and anxiety among 75 AA patients was 66.7% and 73.3%, respectively. About 82.0% had mild depression, 18.0% had moderate depression, and none had severe depression. Further, about 89.0% had mild and 11.0% had moderate anxiety, respectively [31]. Similarly, In another cross-sectional descriptive study performed in Saudi Arabia, the prevalence of alopecia areata was evaluated by distributing a questionnaire among the residents; a total of 5,362 individuals completed the questionnaire and submitted it, with 741 (13.8%) reported having had at least once throughout their lifetimes. The majority were between 11 and 30; AA affected 359 men and 382 women, with 29.4% recovering in less than three months and 59.4% in under a year [32].
In one of the cross-sectional observational studies selected for the review, dermatologists with their Alopecia-affected patients were surveyed in the United States, evaluating the presence of emotional symptoms and effects on daily life activities. The results determined that 242 patients aged 39.2 years were assessed with an average Emotional Symptoms score of 2.0. Average activity impairment and work productivity loss were 12.2% and 13.3%, respectively. Each 1-point increase in ES resulted in an increase in Work Productivity Loss of 4.1% and activity impairment of 3.1%. WPL and activity impairment were significantly decreased [33]. According to a web-based cross-sectional survey in Japan, this study showed the hindrance of alopecia areata on daily activities, such as working productivity. About 45,006 people were selected and questioned about their AA experiences. To check for AA history and quantify the severity of the condition, the Alopecia Assessment Tool and Scalp Hair Assessment PROTM were employed. The most popular form of therapy was topical corticosteroids. However, individuals experienced side effects on their mood, self-worth, and social relationships. The prevalence of people with AA was 43.6%. Nonetheless, patients did not seek treatment, which suggests there is still a need for more therapies, support, or awareness [34].
An online, cross-sectional survey was conducted to measure the severity of Alopecia as a percentage of scalp hair loss in the US population. The Alopecia Assessment Tool (ALTO) and Severity of Alopecia Tool (SALT) were utilised to self-screen as positive for Alopecia and assess the severity of the condition. Participants who self-reported having Alopecia were asked to submit photos for three clinicians to judge if they had Alopecia. The study results indicate that the average age of the participants was 43 years, and (20.4%) uploaded pictures for the clinician's review. The average prevalence of AA as determined by a clinician was 0.21%, 0.12% for “mild” illness, 0.09% for “moderate to severe” illness, and 0.04% for the “moderate to severe” subgroup of alopecia totalis/alopecia universalis. In summary, the average ALT score was 44.4%, with “mild” scoring 8.8% and “moderate to severe” scoring 93.4% [35].
According to another retrospective cross-sectional study held in Saudi Arabia, patients diagnosed with AA were included, and their demographic data were evaluated; the AA type, length of the disease, AA family history, and co-occurring autoimmune disorders of the patients were included. Alopecia totalis, universal, and mild/moderate patches of hairlessness were used to categorize the severity of AA. This study concluded that 2.3% of Saudi patients had Alopecia, with the patchy variety affecting the scalp being the most prevalent [36]. Another prospective cross-sectional study in the United States evaluated the quality of life affected by AA in pediatric patients. The study results indicated that 54% of the patients had mild severity, 24.9% had moderate severity, and 2801% had severe severity [37].
In a long-term follow-up study of AA patients, 104 patients diagnosed with AA were included. The analysis of 104 cases revealed that 88.5% of patients had mild, 3.8% had moderate, and 7.7% had severe AA at the first occurrence. About 74%, 94%, and 100% of patients with childhood genesis, adult genesis, and late-genesis of AA had complete or considerable regrowth. The best cure for the initial incident was systemic steroids. Relapses were common but less frequent with time [38]. According to a study, a qualitative interview was conducted on patients diagnosed with alopecia areata to evaluate the psychological impacts of the disease. According to the Severity of Alopecia Tool (SALT), participants with Alopecia areata (AA) lost 50% of their scalp hair. To find concepts and correlations, data were thematically analysed. Men and women reported the emotional and psychological effects of AA, including sadness or depression, embarrassment or shame, rage or frustration, helplessness or anxiety. Many patients retreated from social situations, damaging bonds and exacerbating isolation [39].
According to a large-scale matched controlled cohort study, in all age groups over 30, anxiety was independently and favorably correlated with AA, with equal rates in men and women. Additionally, depression was independently and favorably correlated with AA, especially in the 30-49 age range, with a stronger correlation among females. Patients with AA are prone to co-occurring mental problems, with female patients and those between the ages of 30-49 being particularly vulnerable [40]. According to another selected study, researchers conducted a cross-sectional investigation on 50 novel childhood atopic dermatitis (AA) cases. Girls had a higher prevalence of AA, with the scalp being the most often affected area. The localised confined patch was the most prevalent appearance, while sisaipho was the least common. Five (10%) of the children had a confirmed family history of AA, 30 had a positive family record of atopy, and 24 had a history of atopic disorders. The most frequent trigger was stress in 13 (26%) participants [41]. A systematic review study determined that depression and anxiety are more common among AA patients. This appears to be especially true for adult patients experiencing more severe hair loss. Younger individuals or those with less severe AA did not correlate significantly with AA, anxiety, or depression [42]. A cross-sectional population-based study determined that adults with Alopecia had bigger numbers of positive PHQ2 and comorbid anxiety and depression than those without Alopecia. There was a correlation between lower patient satisfaction and both positive PHQ2 and positive K6, but not between the percentages of decreased patient satisfaction and comorbid anxiety and depression. This study was conducted on 543 adults with Alopecia in the 2004-2016 Medical Expenditure Panel Survey [43].
According to a case report, a 10-year-old boy consulted a dermatologist regarding patchy hair loss [44]. After the examination, the boy was diagnosed with alopecia areata. The detailed interview revealed that the boy had a variety of symptoms, including anxiety, a desire to sleep with his parents, a dislike of being left alone, loss of appetite and sleep, anguish in response to reminders, and recurrence of symptoms [44]. After peer bullying in school around three months ago, the boy suffered a significant neck injury that made him feel like he would not survive. The first signs of hair loss appeared 5 to 6 weeks after the incident [44]. In another cross-sectional study, the participants were asked about their self-perception, self-esteem, sexual experiences, anxiety, and depressive moods. Females were more affected than males by the negative effects of Alopecia on each psychological measure. In females, only sexual experiences, anxiety, and depression scores were significant; in men, a comparison of all stages of hair loss was significant [45]. All the selected studies and their conclusions can be seen in Table 4.
The diagnosis of alopecia areata is frequently made using the clinical symptoms. Dermoscopy and histology, however, may also be helpful. Alopecia areata medical treatment is very difficult, although recent advances in understanding the molecular pathways have revealed innovative medications and the possibility of remission soon [10].
Table 4.
| S.No | Title | Author | Study | Year | Prevalence | Description |
|---|---|---|---|---|---|---|
| 1 | The psychological impact of alopecia areata. Dermatology research and practice. | Marahatta S, Agrawal S, Adhikari BR. | Cross-sectional Study | 2020 | 66.7% of depression among AA patients. | Cohort studies with a bigger sample size may provide a clearer picture of the link between AA use and its negative psychological effects, such as anxiety and depression. |
| 2 | Prevalence of alopecia areata in Saudi Arabia: a cross-sectional descriptive study. Cureus. | Al-Ajlan A, Alqahtani ME, Alsuwaidan S, Alsalhi A. | Cross-sectional descriptive study | 2020 | 5.2% prevalence of AA patients. | Saudi Arabia has a greater prevalence of AA than Western nations, with men being more afflicted and the mean onset age being lower, suggesting a poorer prognosis. |
| 3 | Alopecia areata: an autoimmune disease of multiple players. Immuno Targets and Therapy. | Suchonwanit P, Kositkuljorn C, Pomsoong C. | Cross-sectional observational study | 2021 | --- | Understanding the underlying processes of AA can help us better understand the pathophysiology and develop more effective treatments. |
| 4 | Prevalence of alopecia areata in Japan: Estimates from a nationally representative sample. | ranishi T, Ito T, Fukuyama M, Isaka Y, Mackie DS, King‐Concialdi K, et al | Cross-sectional prospective study | 2023 | Point prevalence of AA was 2.18%, lifetime prevalence was 5.74%. | There is still a need for further therapies, advocacy, and education in Japan to address the negative effects of AA. |
| 5 | A large cross-sectional survey study of the prevalence of alopecia areata in the United States. | Benigno M, Anastassopoulos KP, Mostaghimi A, Udall M, Daniel SR, Cappelleri JC, et al. | Cross-sectional study | 2020 | 0.12% for “mild” disease, 0.09% for “moderate to severe” disease, and 0.04% for “moderate to severe” subgroup. | The current prevalence of AA in the US is similar to the 1970s, with 0.09% prevalence of “moderate to severe” disease. The burden of AA is considerable due to its impact on quality of life. |
| 6 | Prevalence and clinical characteristics of alopecia areata at a tertiary care center in Saudi Arabia. | Alshahrani AA, Al-Tuwaijri R, Abuoliat ZA, Alyabsi M, AlJasser MI, Alkhodair R | Cross-sectional Study | 2020 | 2.3% prevalence of AA. | Comorbidities, such as hypothyroidism, diabetes mellitus, and atopic diseases were found to be common in AA patients. |
| 7 | The severity of disease and quality of life in parents of children with alopecia areata, totalis, and universalis | Putterman E, Patel DP, Andrade G, Harfmann KL, Hogeling M, Cheng CE, et al. | Prospective cross-sectional study | 2019 | 54%, 24.9% and 28.1% affected with reduced QoL. | Counsellors should adjust their approaches to help parents form reasonable expectations for living with the sickness over the long term. |
| 8 | Alopecia areata: a long‐term follow‐up study of 104 patients. | Lyakhovitsky A, Aronovich A, Gilboa S, Baum S, Barzilai A. | Long-term follow-up study | 2019 | 88.5% mild, 3.8% moderate and 7.7% severe AA. | Increasing age at the beginning has decreased the prevalence of severe illness, length of first episode, and frequency of relapses. |
| 9 | “‘You lose your hair; what is the big deal?’I was so embarrassed; I was so self-conscious, I was so depressed:” a qualitative interview study to understand the psychosocial burden of alopecia areata | Aldhouse NV, Kitchen H, Knight S, Macey J, Nunes FP, Dutronc Y, et al. | Qualitative interview | 2020 | 0.09% From moderate to severe condition. | AA harms patients' relationships, lifestyles, and health; effective therapies and awareness needed. |
| 10 | The association between alopecia areata and anxiety, depression, schizophrenia, and bipolar disorder. | Tzur Bitan D, Berzin D, Kridin K, Cohen A. | Population-based study | 2022 | Positive relation with anxiety and depression | Psychiatric evaluation and care should be provided for AA to reduce psychological distress. |
| 11 | Clinico-epidemiological profile of childhood alopecia areata along with dermoscopic correlation: A cross-section, observational study | Bhardwaj P, Basu D, Podder I, Gharami RC. | A cross-section, observational study | 2021 | 86% of children had moderate illness, 74% had localised confined patches, and 2% had sisaipho. | Female gender, younger age, nail involvement, concurrent atopy, vitiligo, and thyroid dysfunction were insignificant. |
| 12 | Association of mental health outcomes and lower patient satisfaction among adults with Alopecia: A cross-sectional population-based study | Kim AB, Cheng BT, Hassan S | A cross-sectional population-based study | 2022 | 17.9% of AA patients are associated with depression, and 17.3% are associated with anxiety. | Clinicians should modify their approach to help patients with Alopecia and mental health difficulties to increase overall healthcare. |
| 13 | The tendency towards the development of psychosexual disorders in androgenetic Alopecia according to the different stages of hair loss: a cross-sectional study | Tas, B., Kulacaoglu, F., Belli, H., & Altuntas, M. | A cross-sectional study | 2018 | Findings show an increased tendency of pertaining psychosexual disorders in both sexes of AA patients. | Patients may require psychological care depending on the clinical stages of their condition. |
| 14 | Interactions between posttraumatic stress disorder and Alopecia areata in a trauma-exposure child: Two case reports. International Journal of Trichology | Kara, T., & Topkarcı, Z. | case report | 2018 | Positive relation with anxiety and depression. | Psychological burden worsens or enunciates alopecia areata in children. |
| 15 | Association between alopecia areata, anxiety, and depression: a systematic review and meta-analysis | Okhovat J-P, Marks DH, Manatis-Lornell A, Hagigeorges D, Locascio JJ, Senna MM. | a systematic review and meta-analysis | 2019 | Positive association with anxiety and depression. | Healthcare workers should be aware of the increased risk of anxiety in AA Patients. |
CONCLUSION
The examination and evaluation of the 15 selected studies conclude that Alopecia areata is a common immunological disorder that occurs in every age group with different prevalence rates. Children are primarily more affected by the disorder than adults and the elderly. This review indicated that psychological factors, such as mental health, anxiety, stress and depression, play a vital role in causing alopecia areata and can also worsen the disorder. Globally, the prevalence of Alopecia areata is 2%, and its underlying conditions after examinations are hereditary traits or psychological issues. Nonetheless, future research is yet to discover feasible interventions and complications of Alopecia areata.
STRENGTHS AND IMPLICATIONS
The study focuses on studies published between 2018 and 2023, providing an up-to-date understanding of the prevalence and psychological impacts of Alopecia areata. It uses a comprehensive approach, PRISMA criteria and the SPIDER framework to select studies. The study emphasizes the psychological impacts of Alopecia areata, highlighting its impact on quality of life and diverse populations. The study also highlights the importance of Alopecia areata as a non-rare disease with significant implications, challenging misconceptions and promoting better treatment strategies and interventions.
SUGGESTION FOR POLICYMAKERS
- Physicians should routinely assess the psychosocial well-being of patients with AA.
- Incorporating mental health assessments during dermatologic consultations can help identify individuals at risk of anxiety and depression.
- Physicians should integrate mental health care into the overall management of AA
- Policymakers should consider including AA in public health initiatives addressing mental health.
- Policymakers should consider promoting comprehensive care models that integrate psychological support and patient education into routine treatment plans.
LIST OF ABBREVIATIONS
| AA | = Alopecia Areata |
| AU | = Alopecia Universalis |
| AT | = Alopecia Totalis |
| AT | = Alopecia Totalis |
| AO | = Alopecia Ophiasis |
AVAILABILITY OF DATA AND MATERIALS
The authors confirm that the data supporting the findings of this study are available within the article and its supplementary materials.
STANDARDS OF REPORTING
STROBE guidelines were followed.
FUNDING
No organization has funded this study.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
Declared none.
SUPPLEMENTARY MATERIAL
PRISMA checklist is available as supplementary material on the publisher’s website along with the published article.
APPENDICES
| Section and Topic | Item # | Checklist Item | Location where Item is Reported |
|---|---|---|---|
| TITLE | - | ||
| Title | 1 | Identify the report as a systematic review. | 1-4 |
| ABSTRACT | - | ||
| Abstract | 2 | See the PRISMA 2020 for Abstracts checklist. | 22-45 |
| INTRODUCTION | - | ||
| Rationale | 3 | Describe the rationale for the review in the context of existing knowledge. | 49-122 |
| Objectives | 4 | Provide an explicit statement of the objective(s) or question(s) the review addresses. | 120-122 |
| METHODS | - | ||
| Eligibility criteria | 5 | Specify the inclusion and exclusion criteria for the review and how studies were grouped for the syntheses. | 124-192 |
| Information sources | 6 | Specify all databases, registers, websites, organisations, reference lists and other sources searched or consulted to identify studies. Specify the date when each source was last searched or consulted. | 142-156 |
| Search strategy | 7 | Present the full search strategies for all databases, registers and websites, including any filters and limits used. | 131-136 |
| Selection process | 8 | Specify the methods used to decide whether a study met the inclusion criteria of the review, including how many reviewers screened each record and each report retrieved, whether they worked independently, and, if applicable, details of automation tools used in the process. | 175-192 |
| Data collection process | 9 | Specify the methods used to collect data from reports, including how many reviewers collected data from each report, whether they worked independently, any processes for obtaining or confirming data from study investigators, and, if applicable, details of automation tools used in the process. | 175-192 |
| Data items | 10a | List and define all outcomes for which data were sought. Specify whether all results that were compatible with each outcome domain in each study were sought (e.g., for all measures, time points, analyses), and if not, the methods used to decide which results to collect. | 245-289 |
| 10b | List and define all other variables for which data were sought (e.g., participant and intervention characteristics, funding sources). Describe any assumptions made about any missing or unclear information. | --- | |
| Study risk of bias assessment | 11 | Specify the methods used to assess the risk of bias in the included studies, including details of the tool(s) used, how many reviewers assessed each study and whether they worked independently, and if applicable, details of automation tools used in the process. | 231-241 |
| Effect measures | 12 | Specify for each outcome the effect measure(s) (e.g., risk ratio, mean difference) used in the synthesis or presentation of results. | --- |
| Synthesis methods | 13a | Describe the processes used to decide which studies were eligible for each synthesis (e.g., tabulating the study intervention characteristics and comparing against the planned groups for each synthesis (item #5)). | 129-241 |
| 13b | Describe any methods required to prepare the data for presentation or synthesis, such as handling of missing summary statistics or data conversions. | 142-204 | |
| 13c | Describe any methods used to tabulate or visually display the results of individual studies and syntheses. | 292-391 | |
| 13d | Describe any methods used to synthesize results and provide a rationale for the choice(s). If meta-analysis was performed, describe the model(s), method(s) to identify the presence and extent of statistical heterogeneity, and software package(s) used. | --- | |
| 13e | Describe any methods used to explore possible causes of heterogeneity among study results (e.g., subgroup analysis, meta-regression). | --- | |
| 13f | Describe any sensitivity analyses conducted to assess the robustness of the synthesized results. | --- | |
| Reporting bias assessment | 14 | Describe any methods used to assess the risk of bias due to missing results in a synthesis (arising from reporting biases). | --- |
| Certainty assessment | 15 | Describe any methods used to assess certainty (or confidence) in the body of evidence for an outcome. | --- |
| RESULTS | - | ||
| Study selection | 16a | Describe the results of the search and selection process, from the number of records identified in the search to the number of studies included in the review, ideally using a flow diagram. | 194-207 |
| 16b | Cite studies that might appear to meet the inclusion criteria, but which were excluded, and explain why they were excluded. | --- | |
| Study characteristics | 17 | Cite each included study and present its characteristics. | --- |
| Risk of bias in studies | 18 | Present assessments of risk of bias for each included study. | 237-241 |
| Results of individual studies | 19 | For all outcomes, present, for each study: (a) summary statistics for each group (where appropriate) and (b) an effect estimate and its precision (e.g., confidence/credible interval), ideally using structured tables or plots. | 192-207 |
| Results of syntheses | 20a | For each synthesis, briefly summarise the characteristics and risk of bias among contributing studies. | --- |
| 20b | Present results of all statistical syntheses conducted. If meta-analysis was done, present for each the summary estimate and its precision (e.g., confidence/credible interval) and measures of statistical heterogeneity. If comparing groups, describe the direction of the effect. | --- | |
| 20c | Present results of all investigations of possible causes of heterogeneity among study results. | --- | |
| 20d | Present results of all sensitivity analyses conducted to assess the robustness of the synthesized results. | --- | |
| Reporting biases | 21 | Present assessments of risk of bias due to missing results (arising from reporting biases) for each synthesis assessed. | --- |
| Certainty of evidence | 22 | Present assessments of certainty (or confidence) in the body of evidence for each outcome assessed. | --- |
| DISCUSSION | - | ||
| Discussion | 23a | Provide a general interpretation of the results in the context of other evidence. | 209-314 |
| 23b | Discuss any limitations of the evidence included in the review. | --- | |
| 23c | Discuss any limitations of the review processes used. | --- | |
| 23d | Discuss the implications of the results for practice, policy, and future research. | 326-334 | |
| OTHER INFORMATION | - | ||
| Registration and protocol | 24a | Provide registration information for the review, including the register name and registration number, or state that the review was not registered. | --- |
| 24b | Indicate where the review protocol can be accessed or state that a protocol was not prepared. | --- | |
| 24c | Describe and explain any amendments to information provided at registration or in the protocol. | --- | |
| Support | 25 | Describe sources of financial or non-financial support for the review and the role of the funders or sponsors in the review. | 339 |
| Competing interests | 26 | Declare any competing interests of review authors. | 337 |
| Availability of data, code and other materials | 27 | Report which of the following are publicly available and where they can be found: template data collection forms; data extracted from included studies; data used for all analyses; analytic code; any other materials used in the review. | 341-343 |


