All published articles of this journal are available on ScienceDirect.
Cutaneous Pseudolymphoma Secondary to Insect Bite: A Case Report
Abstract
Introduction
Cutaneous Pseudolymphoma (CPL) encompasses a heterogeneous group of benign, reversible, and inflammatory lymphocyte proliferation.
Case presentation
We present a unique instance of CPL triggered by an insect bite in a 42-year-old female who presented to our hospital with a solitary tender erythematous shallow ulcer over her right arm, which was misdiagnosed initially as cutaneous leishmaniasis due to her travel history. A biopsy ultimately revealed cutaneous lymphoid hyperplasia related to an arthropod bite reaction. Moreover, various treatment options were initiated.
Conclusion
This case highlights the need for clinicians to consider CPL in the differential diagnosis of chronic skin lesions to avoid misdiagnosis and ensure appropriate treatment.
1. INTRODUCTION
Cutaneous Pseudolymphoma (CPL) encompasses a heterogeneous group of inflammatory T-cell and B-cell lymphocyte proliferation that is essentially benign and completely reversible. Accordingly, spontaneous remission occurs when an inciting event is identified and eliminated. Several triggers have been suggested as a cause for the disease, such as insect bites, medications, infections, immunizations, genetics, and immunity status. With respect to idiopathic CPL, the course of the disease is considered slow and essentially difficult to treat [1, 2].
The mainstay of diagnosis is clinical presentation along with immunophenotyping. As CPL greatly resembles cutaneous lymphoma, it is of great importance to differentiate between the two [3]. The latter usually presents in a more aggressive manner with multiple large nodules and plaques, while the former presents with fewer and smaller lesions in size and growth [4]. Treatment options are many and diverse; they include excision, which is the preferred modality, in addition to cryotherapy, photodynamic therapy, topicals such as Calcineurin inhibitors and imiquimod, intralesional corticosteroids, or local radiotherapy [2].
This case of cutaneous pseudolymphoma is unique due to its presentation as a solitary, painful ulcer resembling cutaneous leishmaniasis, which initially misled the diagnosis. Additionally, the emergence of contact dermatitis from the application of non- prescribed substances further complicated the treatment course. Therefore, our case highlights the intricacies of diagnosing and treating pseudolymphoma.

2. CASE PRESENTATION
A 42-year-old Filipino female with no clear medical history presented to our dermatology clinic with a 6-month history of a solitary itchy and painful skin lesion over her right upper arm.
Moreover, this pain extended along her whole arm with no swelling or fever, which was aggravated by arm movement. The lesion appeared small and started to enlarge over time, which made the patient seek medical help in another hospital. She was working as a house-made in Jeddah, but she reported that she was bitten by an unknown insect while she was visiting a farm when traveled to Al-Qassim region (400 km northwest of Riyadh), one of the endemic regions of cutaneous Leishmaniasis in Saudi Arabia.
Ketoconazole and Metronidazole were prescribed in another hospital, and the patient noticed slight improvement for a little while. The patient complained of a headache and nausea, which improved after taking analgesics. There were no other systemic symptoms, no other medications used, no smoking history, no known allergies, no trauma or tattoos at the site, no family history of similar lesions, and no history of contact with animals.
A provisional diagnosis of cutaneous leishmaniasis was proposed based on the patient's clinical presentation of visiting an endemic region. Therefore, an empirical systemic oral fluconazole daily and topical clotrimazole with topical antibacterial mupirocin ointment twice per day were prescribed for 1 week. The patient already finished a course of oral amoxicillin/clavulanic acid at the time of presentation from the other hospital, and a blood workup was requested.
Upon examination, a solitary, tender, non-indurated, bright erythematous shallow ulcer was noted over the posterior aspect of the right upper arm. The ulcer measured approximately 6 cm x 3 cm in diameter, with an irregular border and minimal serous discharge. The surrounding skin was erythematous to hyperpigmented (Fig. 1). No swelling or warmth was observed in the arm. The differential diagnosis included cutaneous leishmaniasis versus cutaneous pseudolymphoma secondary to an arthropod (insect) bite reaction. Other differential diagnoses included lymphocytoma cutis, drug reaction, and squamous cell carcinoma.
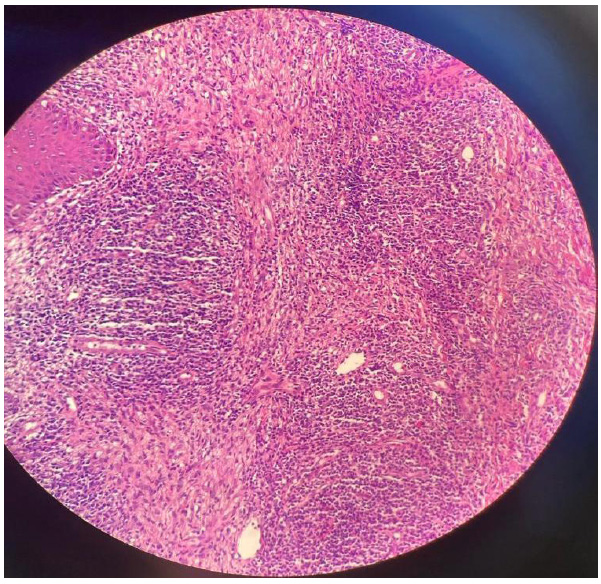
We planned to obtain a baseline 3-mm skin punch biopsy from the edge of the ulcer. Consent was obtained from the patient after explaining the procedure. One week later, the biopsy results revealed a dense perivascular mixed lymphoid infiltrate in both the upper and deep dermis, consistent with cutaneous lymphoid hyperplasia (pseudolymphoma) secondary to an insect bite reaction (Figs. 2A, B).
We discussed the diagnosis with the patient and subsequently discontinued oral fluconazole and topical antifungal treatment. She was started on oral doxycycline 100 mg daily for three weeks, both as an antibacterial and anti-inflammatory agent, along with intralesional corticosteroids (5 mg) administered once every two weeks. This regimen resulted in only partial improvement (Fig. 3). One week later, the patient developed increased redness and pain at the lesion site (Fig. 4). Alternative treatments, such as cryotherapy or other systemic medications, were considered if oral doxycycline and intralesional steroids failed; however, they were not preferred initially due to their potential side effects.

Note: Immunohistochemical staining is not available in our laboratory.
We asked the patient if she applied any non-prescribed material and we found the patient was applying ‘Dates and Myrrh’, which is derived from the Commiphora species, over the lesion, causing contact dermatitis. We instructed her to follow our instructions precisely and not to apply any non-prescribed medicines. A short course of oral prednisolone (30 mg daily) was initiated in combination with doxycycline, the oral antihistamine desloratadine, topical mupirocin ointment, mometasone cream, and Vaseline. After one week, the lesion showed complete resolution with no pain, leaving only residual hyperpigmentation and faint erythema (Fig. 5). Weekly follow-ups were scheduled for two months to review the skin rash improvement clinically and to discuss treatment side effects.



3. DISCUSSION
Cutaneous pseudolymphoma is a benign, reactive lymphoproliferative process that may mimic cutaneous lymphoma clinically and histologically [5]. Pseudolymphoma may have varying presentations from one patient to another [6]. It has a wide spectrum of clinical findings that can be solitary or multiple, grouped or disseminated, plaques or nodules [7, 8]. The initial presentation of our case was a solitary erythematous crusted plaque. Meanwhile, multiple cases have been reported where patients were presented with nodules [2, 9]. Therefore, early identification of pseudolymphoma using clinical, histological, and molecular findings is crucial to reach the proper diagnosis.
There are different approaches to classifying cutaneous pseudolymphoma according to the immunophenotype (T cell, B cells, and mixed), histological pattern, etiology, and clinical findings. Depending on the etiology, pseudolymphoma can be induced by infections, drugs, foreign agents, and others [1]. In young individuals, B. burgdorferi is a common etiology, while medication is more common in adults [2]. The molecular findings for our patient showed an arthropod-bite reaction, which triggered an immune response that led to the patient’s presentation. Furthermore, other cases reported in the literature as pseudolymphoma were secondary to different etiologies, such as leishmania infantum, supplemental flaxseed oil, or drug-induced lamotrigine [4, 10, 11]. However, in other cases, the trigger for pseudolymphoma could not be identified; hence, the term idiopathic cutaneous pseudolymphoma was used [9].
It is important to differentiate pseudolymphoma from other skin lymphomas, which points to the importance of the histological and clinical findings [12]. In our case, the presentation was not specific for pseudolymphoma, and it resembled leishmania, which necessitated the need to perform a biopsy that was crucial to diagnose the patient accurately after the absence of Leishmania in the biopsy. Due to the recent advancements in medicine, there has been progress in the diagnosis of CPL. However, it is still very difficult to distinguish pseudolymphoma from lymphoma, which can pose a serious issue in patient management [13]. The treatment options depend on the causative agent. In cases where the cause can be identified, withdrawal of the instigating agent can be curative. Meanwhile, different therapeutic modalities have been used in idiopathic cases, such as antibiotics, intralesional and systemic steroids, immunotherapy, and excision. Therefore, the therapeutic choice should be individualized for each patient according to the etiology. Moreover, pseudolymphoma can progress to lymphoma if the stimuli persist, which shows the importance of regular monitoring of the patient [14, 15]. Finally, Al-Qassim is not an endemic area for Leishmania, so many cases in the non-endemic area should raise suspicion for cutaneous pseudolymphoma.
CONCLUSION
The term “pseudolymphoma” refers to a wide range of distinct disease subtypes with a broad spectrum of clinical presentations. Therefore, it can be misdiagnosed. This case highlights the need for clinicians to consider CPL in the differential diagnosis of chronic skin lesions to avoid misdiagnosis and ensure appropriate treatment. We hope that our case report on cutaneous pseudolymphoma and other similar cases will help resolve future clinical problems related to the diagnosis.
LIMITATION
The absence of Immunohistochemical Staining (IHC) in our institution, as some markers, can be helpful and sensitive and/or specific in diagnosing cutaneous pseudolymphoma versus cutaneous lymphoma.
AUTHORS’ CONTRIBUTIONS
The authors confirm their contribution to the paper as follows: Study conception and design: AA; draft manuscript: MKA, ASA, and STS. All authors reviewed the results and approved the final version of the manuscript.
LIST OF ABBREVIATIONS
| IHC | = Immunohistochemical Staining |
| CPL | = Cutaneous Pseudolymphoma |
CONSENT FOR PUBLICATION
The authors obtained written consent from the patient for their photographs and medical information to be published.
AVAILABILITY OF DATA AND MATERIAL
All the data and supporting information are provided within the article.
ACKNOWLEDGEMENTS
Declared none.


