All published articles of this journal are available on ScienceDirect.
Patterns and Perceptions of Sunscreen Use in Dermatology vs. Non-dermatology Populations: A Cross-sectional Study
Abstract
Introduction
Sun exposure is a major risk factor for skin cancer and other skin conditions. Sunscreen use remains a significant public health concern. This study examines awareness and attitudes toward sunscreen use, comparing dermatology patients with the non-dermatology population, examining associated factors and usage patterns.
Methodology
A cross-sectional study compared sunscreen use between dermatology patients at the University of Jordan Hospital and the non-dermatology population. An online questionnaire covered sociodemographic factors, skin tone, sun exposure, and sunscreen use, with additional questions for dermatology patients. Statistical analysis included descriptive statistics, chi-square tests, and binary logistic regression.
Results
The study included 1,784 participants, with the majority being females (78.1%) aged 18–24 (51.7%). 75.3% reported using sunscreen, though 42.6% of non-users reported a lack of interest. Women (86.9%), those with higher education (81.7%), and lighter-skinned individuals (84.5%) showed higher usage. Dermatology patients had greater compliance (53.4%) than non-patients.
Discussion
The findings are consistent with regional and international studies showing that females, younger individuals, and those with lighter skin tones are more likely to use sunscreen. Similar to prior research, cost, forgetfulness, and lack of awareness were major barriers to regular use. Dermatology patients showed higher compliance, supporting evidence that professional counseling improves sun-protective behaviors.
Conclusion
Demographic factors significantly influence irregular sunscreen use. Females and younger individuals showed higher usage, while males and older adults were less consistent. Educational level and income also played roles. These findings highlight the need for targeted educational efforts and public health campaigns to improve sunscreen adherence, especially among high-risk groups, contributing to better skin health and cancer prevention.
1. INTRODUCTION
Sun exposure is a well-established risk factor for various dermatological conditions, including skin cancer, premature aging, and other photodermatoses [1-4]. Excessive exposure to ultraviolet radiation (UVR) is a leading cause of skin cancer, with non-melanoma skin cancer (NMSC) being the most commonly diagnosed cancer globally, and cutaneous melanoma remaining a major cause of dermatology-related deaths [5]. According to the World Health Organization (WHO), approximately 132,000 cases of melanoma and three million cases of non-melanoma skin cancer are diagnosed globally each year [6]. Despite this, preventive measures such as sunscreen use and protective clothing are often underestimated, increasing the risk of UV-induced damage [7, 8].
Environmental factors, such as ozone layer depletion, contribute to rising skin cancer rates by allowing more UVR to reach the Earth's surface [9]. Additionally, individual behaviors, including excessive sun exposure and inadequate protective measures, further elevate the risk. Educating the public on these risks and encouraging consistent sun protective habits are crucial steps in reducing skin cancer and other dermatologic conditions.
Consistent application of sunscreen is an essential preventive measure that helps in the reduction of the risks mentioned above [10]. Although awareness of the harmful effects of UVR is growing, sunscreen use continues to be inconsistent, especially in areas with high sun exposure, like Jordan [7]. This inconsistency may be affected by various demographic factors, including age, gender, education level, socioeconomic status, and geographic location.
Dermatology patients might exhibit different behaviors compared to non-patients, due to increased awareness of their dermatological conditions. However, whether this knowledge translates into consistent sunscreen use remains uncertain.
The primary aim of this study is to investigate the role of demographic factors in sunscreen use, among dermatology patients in Jordan compared to non-patients, identifying disparities in sun protection behaviors.
Secondary objectives are to evaluate awareness and attitudes toward sunscreen use in both groups, identify key demographic determinants such as age, gender, education level, socioeconomic status, and geographic location, and examine the frequency and consistency of sunscreen application. Additionally, the study seeks to explore factors contributing to irregular application, providing insights for targeted public health strategies to improve sun protection behaviors.
2. MATERIALS AND METHODS
This cross-sectional observational study investigates differences in sunscreen utilization between dermatology patients at the University of Jordan Hospital (JUH) and non-dermatology patients. A secondary aim is to analyze the influence of demographic factors on sunscreen use to identify awareness, patterns, and variations among different population groups.
Although the study was conducted at a single center (JUH), it is important to note that the hospital serves as a referral center, attracting a diverse patient population from across the country.
The study was conducted in Jordan between August 2024 and January 2025, with its participants drawn from two groups: Dermatology patients at the JUH in Amman, Jordan, and individuals from the general population who were not attending dermatology clinics. Dermatology patients were approached in the outpatient dermatology clinics at JUH during their scheduled visits and invited to participate. The clinic is a general dermatology clinic and provides care for a wide range of medical and cosmetic dermatologic conditions. Non-patients' participants were recruited through an open survey link distributed via social media platforms (e.g., Facebook, Instagram, WhatsApp). All participants accessed and completed the questionnaire online.
The study included male and female participants from both groups, with the exclusion of individuals unable to provide informed consent. Data collection was conducted through an anonymous, easily accessible, and confidential online questionnaire. The questionnaire consisted of five sections: Sociodemographic characteristics (gender, age group, education level, current job, and monthly family income); Skin tone and environmental exposure characteristics; Beliefs, challenges, and perceptions regarding sunscreen use; Sunscreen usage behaviors and practices, and additional questions for the dermatology patient groups regarding their skin conditions and sunscreen use.
It should be clarified that in the questionnaire, specifically in the environmental exposure characteristics section, “Work/Living Environment” indicated whether participants' work or school was conducted indoors or outdoors. “Residential Sun Exposure” referred to the general sunlight level at their place of residence, regardless of the time they personally spent outdoors. “Occupational/Lifestyle Sun Exposure” reflected participants’ perceived sun exposure from work, study, hobbies, or daily activities, which could differ from “Work/Living Environment” (e.g., indoor workers with significant outdoor breaks or activities done in the sun like swimming, running…).
Moreover, in frequency-related questions, the terms 'sometimes' and 'often' were not accompanied by an exact number and were left for participants’ subjective interpretation.
Data preprocessing was performed using OpenRefine (version 3.8.5) to identify inconsistencies and resolve data entry errors. Visualization was carried out in Python (version 3.13) using the Pandas, Matplotlib, and Seaborn libraries.
Descriptive statistics were computed to summarize the study population’s characteristics. Categorical variables were analyzed using chi-square tests to assess associations between independent and dependent variables. Binary logistic regression analysis was conducted in SPSS (version 27) to examine the relationship between predictor variables and sunscreen usage status.
To address multicollinearity, the “under 18 years” category was merged with the “18–24 years” group, and the “less than high school” category was combined with the “high school” group. Model assumptions were evaluated, and statistical significance was set at p < 0.05.
| Sample Characteristics | n | % |
|---|---|---|
| Gender | - | - |
| Female | 1,394 | 78.1 |
| Male | 390 | 21.9 |
| Age Group | - | - |
| Under 18 Years | 45 | 2.5 |
| 18-24 Years | 923 | 51.7 |
| 25-34 Years | 307 | 17.2 |
| 35-44 Years | 228 | 12.8 |
| 45-55 Years | 218 | 12.2 |
| Over 55 Years | 63 | 3.5 |
| Education Level | - | - |
| Less than High School | 47 | 2.6 |
| High School Diploma | 177 | 9.9 |
| College | 226 | 12.7 |
| Bachelor's Degree | 1,187 | 66.5 |
| Master's Degree | 115 | 6.4 |
| Doctoral Degree | 32 | 1.8 |
| Current Job | - | - |
| Unemployed | 442 | 24.8 |
| School Student | 112 | 6.3 |
| University or College Student | 741 | 41.5 |
| Employed | 489 | 27.4 |
| Monthly Family Income | - | - |
| < 500 JD | 347 | 19.5 |
| 500-1500 JD | 592 | 33.2 |
| 1500-2000 JD | 284 | 15.9 |
| > 2000 JD | 561 | 31.4 |
The Institutional Review Board (IRB) of Jordan University Hospital (JUH) in Jordan reviewed and approved the study. The study adhered to the tenets of the Declaration of Helsinki, ensuring ethical standards in design and ongoing monitoring. A brief description of the study’s aim was provided at the beginning of the questionnaire, and informed consent was obtained from all participants. Confidentiality was maintained throughout the study.
3. RESULTS
3.1. Participant Demographics and Characteristics
The study size aimed to include all eligible participants during the recruitment period, ensuring adequate statistical power. The study included 1,784 participants (Table 1 for full sociodemographic factors). The sample was composed predominantly of young adults (51.7% aged 18–24 years; 17.2% 25–34 years) and females (78.1%). Most participants held a Bachelor's degree (66.5%). Current engagement was primarily as students (41.5% university/college; 6.3% school) or employed (27.4%); 24.8% were unemployed. Monthly family income was distributed across brackets: <500 JD (19.5%), 500–1,000 JD (33.2%), 1,500–2,000 JD (15.9%), and >2,000 JD (31.4%).
3.2. Skin and Sun Exposure Characteristics
Participants exhibited diverse skin tones and sun exposure patterns (Table 2). Skin tones were predominantly beige (42.3%), olive (28.9%), or light (22.8%); few reported tanned (5.1%) or dark (0.9%) skin. Most reported primarily indoor work/living conditions (79.3%) and residence in areas of significant (51.1%) or moderate (41.8%) sun exposure; few resided in low-exposure areas (7.2%). Half of the sample reported occupations/lifestyles involving no significant sun exposure (50.1%), while 34.9% had moderate and 15.0% high exposure. Daily sun exposure was typically <2 hours (63.4%; <1 hour: 27.5%, 1-2 hours: 35.9%); fewer reported 2-3 hours (22.7%), 3-4 hours (8.5%), or >4 hours (5.4%).
| Skin and Environmental Factors | n | % |
|---|---|---|
| Skin Tone | - | - |
| Light | 406 | 22.8 |
| Beige | 755 | 42.3 |
| Olive | 516 | 28.9 |
| Tanned | 91 | 5.1 |
| Dark | 16 | 0.9 |
| Work/Living Environment | - | - |
| Mostly Outdoor | 370 | 20.7 |
| Mostly Indoor | 1,414 | 79.3 |
| Residential Sun Exposure | - | - |
| Low | 128 | 7.2 |
| Moderate | 745 | 41.8 |
| High | 911 | 51.1 |
| Occupational/Lifestyle Sun Exposure | - | - |
| Low | 894 | 50.1 |
| Moderate | 622 | 34.9 |
| High | 268 | 15 |
| Daily Sun Exposure Duration | - | - |
| < 1 hour | 490 | 27.5 |
| 1-2 hours | 641 | 35.9 |
| 2-3 hours | 405 | 22.7 |
| 3-4 hours | 151 | 8.5 |
| > 4 hours | 97 | 5.4 |
3.3. Sunscreen Use: Beliefs, Barriers, and Perceptions
Most participants reported sunscreen use as 75.3% (Table 3). Among non-users (24.7%), primary barriers included lack of interest (42.6%), forgetfulness (40.6%), difficulty maintaining regular use (25.4%), and uncomfortable sensation (23.8%). Less frequent barriers involved cost (20.4%), lack of awareness (15.9%), skin sensitivity (12.5%), and difficulty finding suitable products (10.0%); skepticism (e.g., lack of improvement [9.3%], long-term harm [8.6%]) was minimal.
Despite barriers, sunscreen was widely recognized as important for skin protection (90.6% agreed), and 56.1% expressed concern about sun exposure health risks.
Regarding side effects, 34.3% believed that sunscreen had none. Among those reporting concerns, common issues documented were acne (31.4%), skin irritation (24.3%), and hyperpigmentation (22.6%). Other concerns included sweating (20.7%), vitamin D deficiency (11.5%), cancer risk (11.0%), hormonal disruption (4.7%), hirsutism (4.3%), and environmental impacts (3.0%).
| Variable | n | % |
|---|---|---|
| Sunscreen Use | - | - |
| Yes | 1,343 | 75.3 |
| No | 441 | 24.7 |
| Perceived Importance of Sunscreen | - | - |
| Important | 1,616 | 90.6 |
| Not Important | 168 | 9.4 |
| Concerns about Sun Exposure | - | - |
| Concerned | 1,000 | 56.1 |
| A Little Concerned | 519 | 29.1 |
| Unconcerned | 265 | 14.9 |
| Perceived Side Effects | - | - |
| No Side Effects | 612 | 34.3 |
| Acne | 561 | 31.4 |
| Skin Irritation | 434 | 24.3 |
| Hyperpigmentation | 403 | 22.6 |
| Over Sweating | 369 | 20.7 |
| Vitamin D Deficiency | 205 | 11.5 |
| Cancer Risk | 196 | 11.0 |
| Hormone Disruption | 84 | 4.7 |
| Hirsutism | 76 | 4.3 |
| Environmental Impact | 53 | 3.0 |
| Variable | n | % |
| Causes of Not Using Sunscreen (Among Non-Users, n = 441) | - | - |
| Lack of Interest | 188 | 42.6 |
| Forgetfulness | 179 | 40.6 |
| Not Be Able to Comply | 112 | 25.4 |
| Uncomfortable Feeling on the Skin | 105 | 23.8 |
| Cost | 90 | 20.4 |
| Lack of Awareness About its Importance | 63 | 14.3 |
| Skin Sensitivity and Allergies | 55 | 12.5 |
| Difficulty Finding a Sunscreen Suitable Skin Type | 44 | 10.0 |
| Lack of Improvement | 41 | 9.3 |
| Belief in Long-Term Harmfulness | 38 | 8.6 |
| Due to Side Effects | 23 | 5.2 |
| Sunscreen Usage Characteristics | n | % |
|---|---|---|
| Frequency of Sunscreen Application Before Sun Exposure | - | - |
| Sometimes | 303 | 22.6 |
| Often | 394 | 29.3 |
| Always | 646 | 48.1 |
| Preferred SPF Level | - | - |
| SPF 15 | 80 | 6.0 |
| SPF 30 | 201 | 15.0 |
| SPF 50 | 434 | 32.3 |
| SPF 50+ | 628 | 46.8 |
| Daily Sunscreen Application Amount | - | - |
| Not Applied Daily | 121 | 9.0 |
| Just a Little Bit (15-25 ml) | 548 | 40.8 |
| Moderate Amount (25-35 ml) | 630 | 46.9 |
| A Lot (>35 ml) | 44 | 3.3 |
| Sunscreen reapplication frequency (especially after swimming or sweating) | - | - |
| Never | 254 | 18.9 |
| Rarely | 353 | 26.3 |
| Sometimes | 448 | 33.4 |
| Always | 288 | 21.4 |
| Sunscreen Application Method | - | - |
| Directly From the Bottle | 1,234 | 91.9 |
| Sprayed On | 70 | 5.2 |
| Applied by Someone Else | 39 | 2.9 |
| Sunscreen Removal Method | - | - |
| Soap and Water | 608 | 45.3 |
| Makeup Remover | 414 | 30.8 |
| Usually Do Not Remove Sunscreen | 268 | 20.0 |
| Specialized Sunscreen Remover | 31 | 2.3 |
| Face Cleanser | 22 | 1.6 |
| Sunscreen Usage Characteristics | n | % |
| Body Areas Where Sunscreen Is Applied | - | - |
| Face | 1,279 | 54.6 |
| Hands | 520 | 22.2 |
| Neck | 321 | 13.7 |
| Arms | 104 | 4.4 |
| Forearms | 69 | 2.9 |
| Chest | 22 | 0.9 |
| Whole Body | 16 | 0.7 |
| Back | 13 | 0.6 |
| Factors Affecting Sunscreen Choice | - | - |
| Brand Reputation | 809 | 60.2 |
| SPF Level | 800 | 59.6 |
| Price | 634 | 47.2 |
| Healthcare Professional Recommendation | 538 | 40.1 |
| Ingredients | 324 | 24.1 |
| Water Resistance | 222 | 16.5 |
| Packaging and Design | 59 | 4.4 |
| Occurred Side Effects | - | - |
| No Side Effects | 751 | 55.9 |
| Acne | 327 | 24.3 |
| Over Sweating | 172 | 12.8 |
| Skin Irritation | 155 | 11.5 |
| Hyperpigmentation | 122 | 9.1 |
| Vitamin D Deficiency | 58 | 4.3 |
| Hirsutism | 35 | 2.6 |
| Hormone Disruption | 20 | 1.5 |
| Environmental Impact | 12 | 0.9 |
3.4. Sunscreen Use Patterns and Practices among Users
Among sunscreen users (n = 1,343), nearly half (48.1%) reported “always” applying sunscreen when anticipating sun exposure; 29.3% applied “often” and 22.6% “sometimes” (Table 4). Sun Protection Factor (SPF) 50+ (46.8%) or SPF 50 (32.3%) were used by most; fewer used SPF 30 (15.0%) or SPF 15 (6.0%).
Application quantity was typically moderate (25–35 ml: 46.9%) or small (15–25 ml: 40.8%); few used >35 ml (3.3%) or applied non-daily (9.0%). The face was the primary application site (95.2%); hands (38.7%) and neck (23.9%) were secondary, while other body areas were rarely covered (<8%). Most were applied directly from the bottle (91.9%).
Participants were asked whether they usually reapply sunscreen throughout the day, particularly after swimming or sweating. Reapplication was inconsistent: only 21.4% “always” reapplied, while 33.4% did “sometimes,” 26.3% “rarely,” and 18.9% “never.” Removal methods varied: soap and water (45.3%), makeup removers (30.8%), specialized removers (2.3%); notably, 20.0% reported no regular removal.
Key choice factors were brand reputation (60.2%), SPF level (59.6%), price (47.2%), and HCP recommendations (40.1%); other factors (ingredients, water resistance, packaging) were less influential (<25%). Most users (55.9%) reported no side effects; among those experiencing effects, acne (24.3%), sweating (12.8%), irritation (11.5%), and hyperpigmentation (9.1%) were most common.
3.5. Associations between Demographic Characteristics, Sunscreen Beliefs, and Sunscreen Use
Gender showed a pronounced association with sunscreen use (χ2(1) = 466.17, p < .001), with significantly higher usage among females (86.9%) than males (33.6%) (Fig. 1). Age was significantly associated with use (χ2(5) = 24.00, p < .001), highest among those aged 45–55 (78.4%) and lowest among those over 55 years (50.8%). Education showed a significant association (χ2(5) = 30.60, p < .001), with higher use among individuals with Master’s (81.7%) or Doctorate degrees (81.3%) compared to those without a high school diploma (53.2%). Skin tone was significantly associated with use (χ2(4) = 30.60, p < .001), highest among individuals with lighter skin tones (Tone 1: 84.5%) and lower among those with tanned (Tone 4: 50.5%) or dark skin (Tone 5: 62.5%).
Agreement with the importance of sunscreen use was strongly associated with higher usage rates (Agreed: 80.2% vs. Disagreed: 28.0%; χ2(1) = 223.02, p < .001). Greater concern about sun exposure health risks predicted higher use (Concerned: 85.5%, Mildly Concerned: 69.7%, Unconcerned: 47.5%; χ2(2) = 174.18, p < .001). A small but significant association was observed with beliefs about side effects (Believed no side effects: 78.4% vs. Believed side effects: 73.6%; χ2(1) = 4.97, p = .026). Usage varied by daily sun exposure duration (χ2(4) = 22.80, p < .001), highest among those exposed for 3–4 hours daily (84.3%) and lowest among those with less than 1-hour exposure (72.0%).
No significant associations were found with family income (χ2(3) = 6.84, p = .077), work environment (indoor/outdoor) (χ2(1) = 3.36, p = .067), residential sun exposure (χ2(2) = 1.59, p = .452), or occupational/lifestyle sun exposure (χ2(2) = 5.26, p = .072).
3.6. Demographic and Perceptual Factors Influencing Sunscreen Use among Users
Gender showed a strong association with sunscreen use frequency (χ2(2) = 77.99, p < .001). Females were more likely to report “always” using sunscreen (51.2%) compared to males (19.1%), who more frequently reported “sometimes” use (51.1% vs. 19.5% in females) (Fig. 2). Age was significantly associated with use frequency (χ2(10) = 20.55, p = .024), with higher consistent use among younger adults aged 18–24 (50.8%) and 25–34 (48.9%), and lower among individuals <18 (29.4%) and >55 (28.1%). The linear trend was not significant (p = .212), suggesting a non-monotonic relationship. Skin tone showed significant differences in use frequency (χ2(8) = 17.77, p = .023) with a significant linear trend (p < .001). Consistent use was highest among lighter tones (Tone 1: 54.2%, Tone 2: 47.7%) and lowest among darker tones (Tone 4: 28.3%, Tone 5: 30.0%).
Education was significantly associated with use frequency (χ2(10) = 18.30, p = .049), and it showed a strong linear trend (p < .001). Higher education levels were linked to greater consistent use, with those holding a Master's (53.2%) or Doctorate (50.0%) reporting higher “always” use compared to those with less than high school education (36.0%) or only high school education (33.9%). Believing sunscreen is important was associated with significantly higher consistent use (Agreed: 49.3% “always” vs. Disagreed: 14.9%; χ2(2) = 37.45, p < .001). Concerns about sun exposure risks predicted greater consistent use (Concerned: 53.8% “always” vs. Mildly Concerned: 37.0%, Unconcerned: 41.3%; χ2(4) = 36.84, p < .001; linear trend p < .001). Those believing sunscreen has no side effects reported higher consistent use (56.7% “always”) than those who believed it has side effects (43.3%; χ2(2) = 22.45, p < .001). Participants without prior side effects reported higher consistent use (51.1% “always”) compared to those who had experienced side effects (44.3%; χ2(2) = 8.86, p = .012).
No significant associations were found with monthly family income (p = .121), work or lifestyle environment (p = .656), residential sun exposure (p = .629), occupational/lifestyle sun exposure (p = .785), or daily sun exposure duration (p = .258).
3.7. Sunscreen Application and Compliance among Dermatology Clinic Patients
A total of 22.4% (n = 400) of participants were current dermatology clinic patients, of whom 54.8% (n = 219) reported having a dermatological diagnosis (Table 5). Among these, acne (59.2%) and eczema (24.8%) were the most common conditions. Other diagnoses, including hives, rosacea, psoriasis, and vitiligo, were each reported by fewer than 11% of patients. Only 48.9% of diagnosed individuals reported “always” applying sunscreen specifically for their condition.
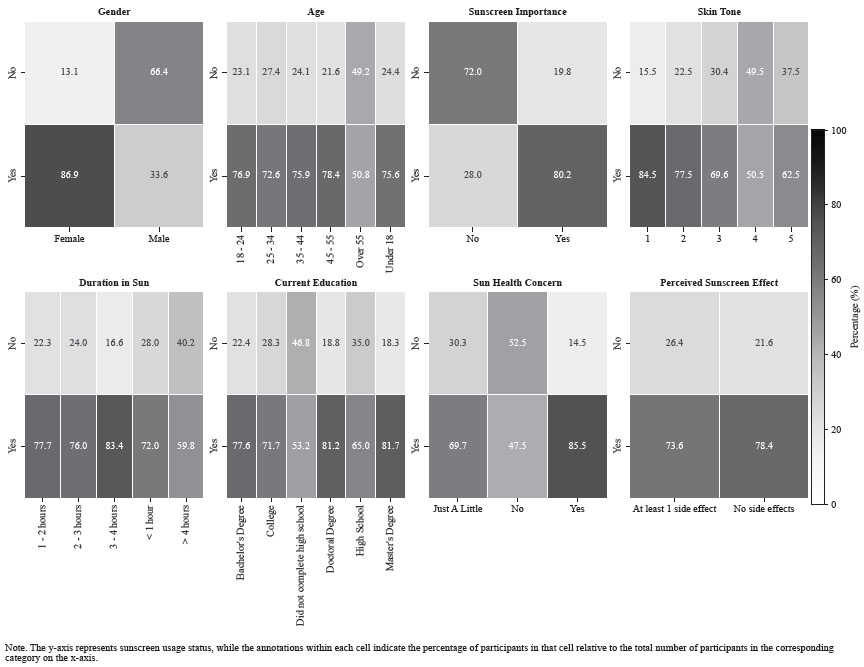
Heatmap analysis of demographic and behavioral factors influencing sunscreen usage status.
| Dermatology-Related Questions | n | % |
|---|---|---|
| Current Dermatology Patient | - | - |
| Yes | 400 | 22.4 |
| No | 1,384 | 77.6 |
| Diagnosed with Dermatological Condition (Among Current Dermatology Patients, n = 400) | - | - |
| Yes | 219 | 54.8 |
| No | 181 | 45.3 |
| Specified Dermatological Condition(s) (Among Those Diagnosed, n = 219) | - | - |
| Acne | 129 | 58.9 |
| Eczema | 54 | 24.7 |
| Hives | 23 | 10.5 |
| Rosacea | 22 | 10 |
| Psoriasis | 14 | 6.4 |
| Vitiligo | 8 | 3.7 |
| Warts | 4 | 1.8 |
| Fungal Infection | 2 | 0.9 |
| Others | 4 | 1.8 |
| Sunscreen Use for Condition Management (Among Those Diagnosed, n = 219) | - | - |
| Never | 30 | 13.7 |
| Rarely | 30 | 13.7 |
| Sometimes | 52 | 23.7 |
| Always | 107 | 48.9 |
| Predictor | B (S.E.) | OR [95% CI] | p-value |
|---|---|---|---|
| Gender (Females vs. Males) | 2.42 (0.16) | 11.21 [8.26, 15.21] | < .001 |
| Perceived Importance (Important vs. Not) | 1.58 (0.24) | 4.85 [3.05, 7.71] | < .001 |
| Concerned About Health Risks of Sun | |||
| Just a little vs. No | 0.42 (0.20) | 1.52 [1.02, 2.26] | .039 |
| Yes vs. No | 1.03 (0.20) | 2.79 [1.90, 4.12] | < .001 |
| Dermatology Patient (Yes vs. No) | 0.40 (0.18) | 1.50 [1.05, 2.13] | .024 |
| Perceived Side Effects (No vs. Yes) | 0.33 (0.15) | 1.39 [1.03, 1.87] | .033 |
| Age (25-34 years vs. ≤ 24 years) | - 0.27 (0.20) | 0.76 [0.52, 1.12] | .171 |
| Age (35-44 years vs. ≤ 24 years) | - 0.15 (0.23) | 0.86 [0.55, 1.34] | .495 |
| Age (45-55 years vs. ≤ 24 years) | 0.15 (0.24) | 1.16 [0.73, 1.84] | .536 |
| Age (Over 55 years vs. ≤ 24 years) | - 0.93 (0.34) | 0.40 [0.20, 0.78] | .007 |
| Current Education Level | |||
| College vs. High School | 0.21 (0.26) | 1.23 [0.74, 2.10] | .427 |
| Bachelor's Degree vs. ≤High School | 0.49 (0.21) | 1.63 [1.08, 2.45] | .021 |
| Master's Degree vs. ≤High School | 0.99 (0.36) | 2.7 [1.34, 5.43] | .005 |
| Doctoral Degree vs. ≤High School | 1.73 (0.62) | 5.61 [1.68, 18.79] | .005 |
| Daily Sun Exposure Duration | |||
| 1-2 hours vs. <1 hour | 0.54 (0.18) | 1.71 [1.20, 2.42] | .003 |
| 2-3 hours vs. <1 hour | 0.50 (0.21) | 1.64 [1.08, 2.49] | .020 |
| 3-4 hours vs. <1 hour | 0.94 (0.33) | 2.57 [1.35, 4.87] | .004 |
| ≥4 hours vs. <1 hour | - 0.10 (0.35) | 0.91 [0.46, 1.81] | .784 |
| Predictor | B (S.E.) | OR [95% CI] | p-value |
| Skin Tone (Beige vs. Light) | - 0.41 (0.20) | 0.67 [0.45, 0.98] | .038 |
| Skin Tone (Olive vs. Light) | - 0.41 (0.21) | 0.66 [0.44, 0.99] | .049 |
| Skin Tone (Tanned vs. Light) | - 0.62 (0.33) | 0.54 [0.28, 1.02] | .057 |
| Skin Tone (Dark vs. Light) | 0.46 (0.18) | 1.58 [0.37, 6.84] | .539 |
| Monthly Family Income | |||
| 500-1500 JD vs. <500 JD | 0.05 (0.20) | 1.05 [0.70, 1.56] | .819 |
| 1500-2000 JD vs. <500 JD | 0.14 (0.25) | 1.15 [0.71, 1.87] | .560 |
| >2000 JD vs. <500 JD | 0.01 (0.21) | 1.01 [0.66, 1.52] | .980 |
| Residential Sun Exposure | |||
| Moderate vs. Low | - 0.29 (0.29) | 0.75 [0.42, 1.33] | .329 |
| High vs. Low | - 0.39 (0.29) | 0.68 [0.38, 1.20] | .180 |
| Lifestyle Sun Exposure | |||
| Moderate vs. Low | 0.27 (0.17) | 1.32 [0.95, 1.83] | .104 |
| High vs. Low | 0.38 (0.25) | 1.46 [1.08, 2.49] | .132 |
| Work Environment | |||
| Mostly Outdoor vs. Mostly Indoor | - 0.14 (0.19) | 0.87 [0.60, 1.26] | .453 |
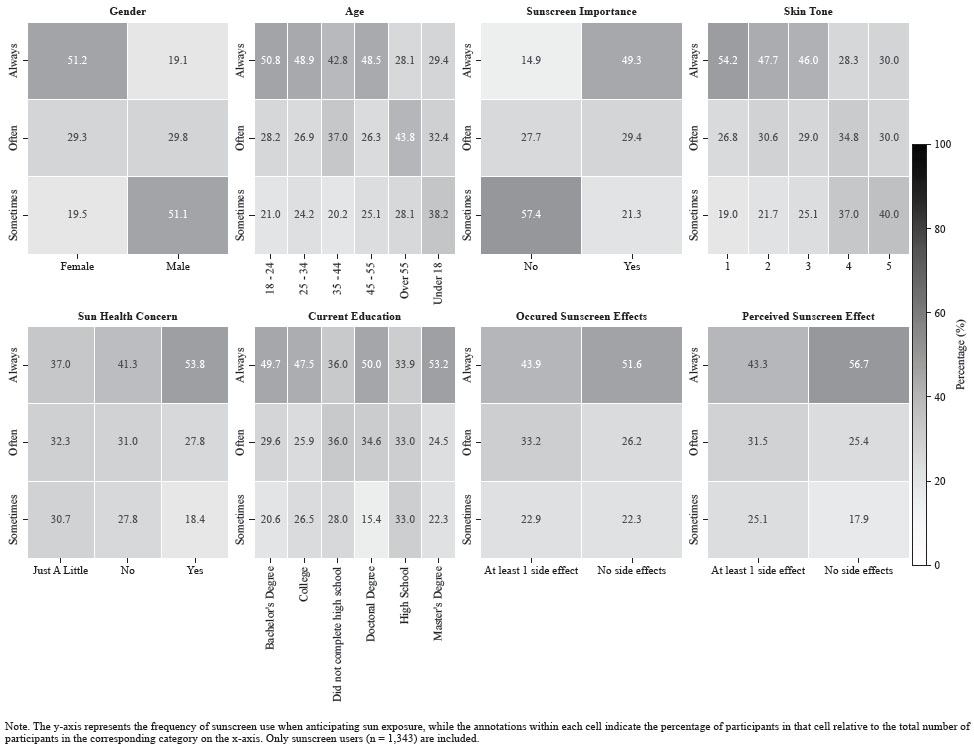
Heatmap Analysis of Demographic and Behavioral Factors Influencing Frequency of Sunscreen Usage.
Dermatology patients exhibited significantly better sunscreen compliance than non-patients (Fig. 3). In terms of frequency, more dermatology patients “always” used sunscreen when anticipating sun exposure (53.4% vs. 46.4%; χ2(2) = 6.74, p = .034). For the daily amount, more patients applied a moderate amount (25–35 ml: 55.6% vs. 44.2%) and fewer applied sunscreen non-daily (4.7% vs. 10.4%; χ2(3) = 19.07, p < .001). Regarding reapplication, more patients reported “always” reapplying sunscreen (27.8% vs. 19.5%; χ2(3) = 13.15, p = .004). For removal practices, fewer patients reported not removing sunscreen at all (12.5% vs. 22.3%), while more used specialized removers (4.1% vs. 1.8%; χ2(4) = 19.13, p < .001). No significant difference was observed in SPF level preference (χ2(3) = 4.31, p = .230).
3.8. Factors Associated with Sunscreen Usage: Results from a Logistic Regression Analysis
The logistic regression model significantly predicted sunscreen use (χ2(30) = 624.24, p < .001) with adequate fit (Hosmer-Lemeshow p = .122) and no multicollinearity (VIFs < 10). The model explained 44% of the variance (Nagelkerke R2) and correctly classified 84.6% of cases (Table 6).
Gender was a strong predictor, with females having 11 times higher odds of sunscreen use compared to males (OR = 11.21, p < .001). Belief in the importance of sunscreen was associated with significantly higher use (OR = 4.85, p < .001), as was concern about sun exposure risks (OR = 2.79, p < .001). Belief in the absence of side effects was also predictive (OR = 1.39, p = .033).
Older age was associated with lower use, with participants >55 years having reduced odds compared to those aged 18–24 (OR = 0.30, p = .007). Higher education predicted greater use, particularly among those with a Doctoral degree (OR = 5.61, p = .005) compared to those with a high school diploma or less.
Daily sun exposure showed a progressive association: 1–2 hours (OR = 1.71, p = .003), 2–3 hours (OR = 1.64, p = .020), and 3–4 hours (OR = 2.57, p = .004), compared to less than 1 hour. Skin tone also played a role, with lower odds among beige (OR = 0.67, p = .038) and olive skin tones (OR = 0.66, p = .049) relative to light skin. Dermatology patients had significantly higher odds of sunscreen use than non-patients (OR = 1.50, p = .024).
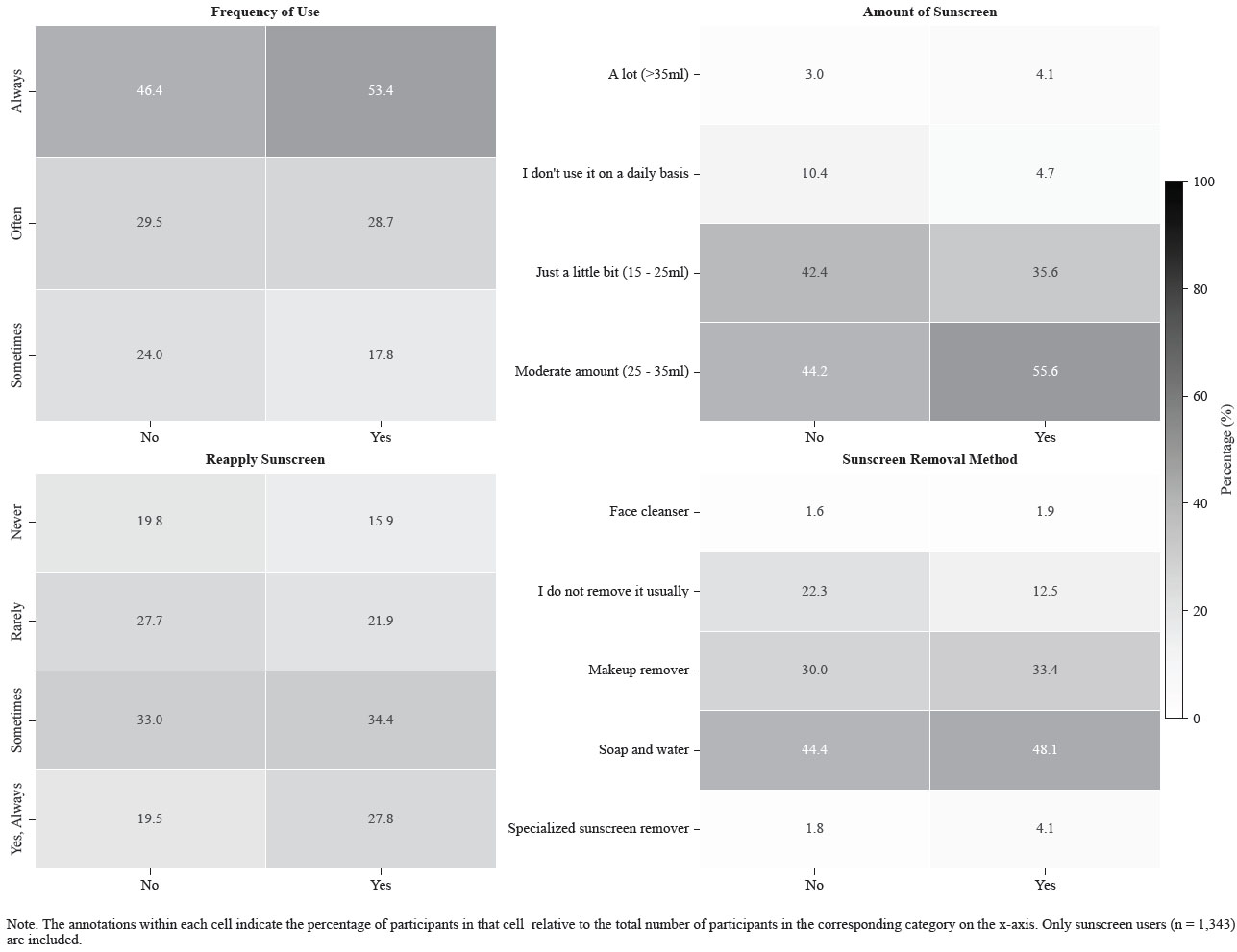
Association between dermatology clinic visits and sunscreen usage patterns.
4. DISCUSSION
This cross-sectional study assessed sunscreen use among dermatology patients and the non-dermatology population in Jordan, focusing on awareness, application habits, and the influence of demographic factors. The findings provide key insights into sun protection behaviors, highlighting disparities in sunscreen adherence, preferred SPF levels, application patterns, and the impact of factors such as skin tone, sun exposure, and lifestyle. Additionally, this study identifies the barriers associated with consistent sunscreen use, offering valuable information for future public health interventions aimed at improving sun protection practices.
Sun protection behaviors have been shown to be extremely influenced by participants’ skin type, as well as sun exposure characteristics. A significant portion of the participants had beige (42.3%) or olive (28.9%) complexion, whereas the darker skin tones were underreported. This is supported by another study done in Jordan, which also highlighted the fact that individuals with darker skin tones underestimate the importance of sunscreen application [9].
Participants with lighter skin tones, who are more aware of the fact that they are more susceptible to sunburn and skin damage, used sunscreen more than participants with darker skin tones who believe they are at a lower risk for sun-related damage, despite evidence indicating they can still develop skin cancer and pigmentation disorders [11]. In addition, lighter skin is sometimes culturally preferred, which can encourage sunscreen use among certain groups in Jordan. These indoor lifestyles were reported as being 79.3%, reducing sunlight exposure and, as a result, reducing the use of sunscreen application habits. This correlates with the results of another study, which mentioned that individuals with indoor lifestyles would usually play a vital role in decreasing the use of sunscreen, as it is not considered necessary [10]. However, 51.1% of the participants live in areas with significant sun exposure, indicating that extra sun protection measures are necessary.
Although many have reported occupations or lifestyles (50.1%) that limit their sunlight exposure, others experience high exposure to sunlight (15%), proving that sun protection habits differ based on individual exposure levels.
Moreover, most of the participants (63.4%) reported less than two hours of daily sunlight exposure. This may also influence sunscreen use habits, as individuals with less exposure would not consider sunscreen application as a priority. 66.9% of the female participants have reported wearing the hijab, which would provide some extent of sun protection while also influencing the consistency of using sunscreen. This was also briefly mentioned in another study portraying that cultural factors also play a role in sunscreen application [9].
Various trends in sunscreen application behaviors have been reported in this study. Although a huge portion of the participants (75.3%) use sunscreen, the number of participants who applied it before sunlight exposure was only 48.1%. This is supported by another study, which also showed that the number of individuals who would apply sunscreen before exposure was less than 50% [10]. This huge variety in responses indicates gaps in sunscreen application adherence, which are usually due to many reasons, including cost obstacles, misunderstandings about the necessity of sunscreen use, or simply forgetfulness. This was also proven in another study that mentioned cost, lack of knowledge, and forgetfulness as obstacles to the use of sunscreen [12]. Most participants (46.8%) reported SPF 50+ preference, and 32.3% reported SPF 50 preference, which portrays general awareness about the vital role of higher sun protection factors. Another study also confirmed that most individuals prefer higher SPF levels of SPF 30 and above [13]. This aligns with the dermatological guidelines published to date around the use of sunscreen [14]. However, it was concluded through the survey that the application quantity varied, with 40.8% of participants using only a small amount of sunscreen, which would also play a huge role in reducing its effectiveness.
A narrow distribution of sunscreen has been suggested by the fact that most participants (95.2%) applied sunscreen exclusively to the face. Most research papers reported similar findings. One study indicated that the body regions receiving the best coverage were the face and neck, with median missed areas of less than 6% after a single application and less than 2% after a double application [15]. Nevertheless, a portion of participants have reported applying sunscreen to their hands (38.7%), whereas another group (23.9%) applied sunscreen to their neck, which is also considered an area regularly exposed to sunlight. Since participants are choosing to protect only some areas of their body, incomplete sun protection remains a concern. Moreover, a major problem stems from the fact that only 21.4% of the participants regularly reapplied sunscreen, although proper protection requires reapplication, especially in certain situations involving sweating or swimming. It was also mentioned in another study that although some individuals are more exposed to sunlight, the number of individuals who reapply sunscreen was limited. The vast majority of users (91.9%) applied sunscreen directly from the bottle, while smaller proportions used spray (5.2%) or received assistance from another person (2.9%) [16].
In addition, this study examined many factors that influenced the selection of sunscreen, including brand reputation (60.2%) and SPF level (59.6%), which were considered the most important factors. Other factors, such as price (47.2%) and healthcare professionals’ recommendations (40.1%), were proven to also play a vital role in influencing participants’ purchasing decisions. Another study also mentioned the factors that influence sunscreen use, such as recommendations from healthcare professionals and brand reputation, as well as SPF levels [17]. Another study showed that other factors, such as texture, water resistance, ingredients, and broad-spectrum protection, were selected slightly less frequently [18]. Some participants reported side effects from the use of sunscreen, with the most significant ones being acne (24.3%) and skin irritation (11.5%). This is supported by another study that highlights dry skin, acne, and irritation as side effects reported by individuals [19]. In a cross-sectional study by Agarwal, the most common side effects were also acne (31%), followed by skin irritation (29%) [20].
Sunscreen is a well-known protective measure against UVR, helping to reduce the risk of sunburn, premature aging, and skin cancer. However, its usage varies significantly across different populations due to a variety of sociodemographic and behavioral factors. Understanding these influences is essential for developing targeted public health campaigns to improve adherence to sunscreen use.
This study highlights the need for increased patient education on proper UV protection. Nearly half of the participants (48.1%) could correctly identify the recommended frequency of sunscreen application and the minimum suggested SPF (46.8%) for daily use. However, overall, only 29.3% of users applied sunscreen “often,” and 22.6% applied it “sometimes.” This finding aligns with another study conducted in Saudi Arabia, which indicated that 57% of participants used sunscreen regularly [21].
Regarding SPF levels, the majority of participants (46.8%) preferred SPF 50+, followed by SPF 50 (32.3%), SPF 30 (15%), and SPF 15 (6%). These results align with findings from various published studies, particularly a cross-sectional study indicating that more than two-thirds of patients choose sunscreens with the highest SPF [21].
In terms of daily application quantity, 46.9% reported using a moderate amount of sunscreen (25–35 ml), while 40.8% applied only a small amount (15–25 ml). A smaller proportion (3.3%) used a large amount (more than 35 ml), and 9% indicated that they do not apply sunscreen daily. This contrasts with findings from the USA, which show that a higher percentage of people (45.4%) apply more than 30 ml of sunscreen [16].
In the non-using group, the primary reasons given for not using sunscreen were a lack of interest (42.6%), forgetfulness (40.6%), and a perceived inability to maintain consistent use (25.4%). Previous studies have also highlighted additional reasons for not using sunscreen, such as experiencing burning and stinging sensations in the eyes [22-24], unpleasant smells associated with its use, high costs [25], and forgetfulness [23, 24]. A study conducted in Portugal identified similar barriers, noting that the properties of sunscreen, its cost, and forgetfulness were the main reasons for non-use [26]. Additionally, some individuals expressed concerns that using sunscreen could lead to vitamin D deficiency [27].
This study examined sunscreen application habits and compliance among dermatology clinic patients versus non-patients, revealing that those with dermatological care demonstrated significantly better sun protection behaviors across multiple domains. These findings are consistent with prior research and provide new insights into patient compliance and educational gaps [13, 27].
Dermatology clinic patients were significantly more likely to report always using sunscreen (53.4%) compared to non-patients (46.4%), suggesting greater awareness and behavior reinforcement. These findings align with Holman et al. [13], who found that individuals who had recently visited a dermatologist were more likely to use sunscreen regularly, reflecting the influence of professional advice. Draelos (2001) [28] similarly emphasized the impact of dermatologist counseling on compliance with skincare routines, including sunscreen use. Another study emphasizes that dermatology visits often provide opportunities to reinforce sun protection, especially for individuals managing chronic skin conditions [29].
This study also found that dermatology patients applied sunscreen in more appropriate quantities and were more diligent in reapplying it throughout the day than non-patients. Over half of the sample (55.6%) reported using a moderate amount (25–35 ml) of sunscreen, consistent with the American Academy of Dermatology’s (2023) guideline recommending approximately one ounce (30 ml) per full-body application [30]. These behaviors are crucial for effective UV protection, as previous research highlighted that insufficient application can reduce sunscreen efficacy, even with high SPF ratings [31].
Despite better compliance in usage and reapplication, there was no significant difference in the SPF level used between the two groups. This suggests that while dermatology patients may be more consistent in sunscreen use, the qualitative aspect of their choices (e.g., selecting high SPF) is not necessarily superior. This finding partially contrasts with a study that noted individuals receiving sun safety counseling were more likely to choose sunscreens with SPF 30 or higher [32].
A novel finding in this study is the significantly higher rate of sunscreen removal among dermatology patients. Only 12.5% failed to remove sunscreen at the end of the day, compared to 22.3% of non-patients. This behavior may be driven by the presence of underlying skin conditions, such as acne and eczema, where proper removal reduces the risk of irritation or flare-ups. A study noted that failure to remove sunscreen could contribute to clogged pores and dermatitis in sensitive individuals [33].
The higher compliance seen among dermatology patients underlines the critical role of clinical visits in promoting sun-safe behaviors. However, the lack of significant differences in SPF level indicates an opportunity for improved education during dermatologic consultations. Standardizing guidance not only on sunscreen use, but also on the appropriate type and proper removal, may improve patient outcomes. Furthermore, integrating visual aids, reminders, or even app-based interventions could reinforce sunscreen habits between visits [34].
The logistic regression analysis revealed several key demographic, behavioral, and perceptual predictors of sunscreen usage. The model demonstrated a good fit and high classification accuracy (84.6%), underscoring the strength of these associations and indicating that sunscreen behavior is influenced by a complex interplay of individual factors. Gender was the strongest predictor of sunscreen use, with female participants showing over 11 times higher odds of using sunscreen compared to males. This is consistent with the cultural norms in Jordan that tend to influence men to avoid products perceived as cosmetics, which may contribute to lower sunscreen use. This finding is consistent with previous research, which indicates that women are more likely to engage in sun-protective behaviors due to their greater concern about skin aging and appearance, as well as a higher overall awareness of health [13, 35].
Perceptions of sunscreen's importance in preventing skin damage significantly increased the likelihood of its use. This aligns with health behavior theories such as the Health Belief Model, which emphasizes perceived benefits and threats as key motivators. Additionally, concern about sun-related health risks, like skin cancer, was a strong positive predictor of sunscreen use, reinforcing findings that risk perception is a major driver of sun protection practices [36]. Participants who did not experience side effects from sunscreen were more likely to use it, although the effect size was modest. Previous studies have shown that concerns over greasiness, breakouts, or allergic reactions can hinder regular sunscreen use [28]. Educating individuals on how to select appropriate formulations for their skin type may help mitigate these barriers.
Older adults were significantly less likely to use sunscreen than their younger counterparts. This trend is paradoxical, given the cumulative nature of UV damage, but it is consistent with prior research, which indicates that older adults often underestimate their susceptibility to sun damage or prioritize other health concerns [37]. In Jordan, this may be related to the limited sun safety campaigns and awareness in earlier decades.
Educational attainment was positively associated with sunscreen use, with the highest levels of usage observed among individuals with doctoral degrees. This trend likely reflects an increase in health literacy and better access to preventive health information among those with higher education [38].
Sunscreen use also increased with greater daily sun exposure, particularly in the 1-4 hour range. This may indicate a threshold at which individuals recognize the necessity of sun protection. Similar patterns have been documented in studies showing that perceived UV exposure influences compliance with sun safety recommendations [39].
These findings underscore the need for targeted public health interventions that address misconceptions, improve accessibility, and personalize sun safety education, particularly for high-risk groups such as men, older adults, and individuals with darker skin tones.
Several limitations must be acknowledged in this study. First, the cross-sectional design studies sunscreen behaviors and attitudes at a single point in time, making it difficult to find the relationship between demographic factors and sunscreen use. Additionally, while JUH is a major referral hospital attracting a diverse patient base, it is a single center, so sampling bias is possible and may limit generalizability. In addition, the online non-dermatology population sample showed a marked overrepresentation of young, highly educated women, reflecting coverage and volunteer bias toward internet-connected, health-aware users.
Another limitation is the reliance on self-reported data, which may cause recall or social desirability bias. Also, the predominance of young, highly educated female participants may have influenced the results, potentially over-representing sunscreen use behaviors compared to a more gender-balanced or older population. Furthermore, distributing the questionnaire online for the non-dermatology population group may have restricted participation to individuals with internet access and higher health awareness.
Also, the subjective interpretation of frequency terms such as ‘sometimes’ and ‘often’ may have introduced variability in responses. Moreover, the questionnaire did not assess whether sunscreens provided UVA protection; only SPF (UVB protection) was recorded, limiting evaluation of full protection. Regardless, this study provides valuable insights into sunscreen use behaviors and the influence of demographic factors and being dermatology patients or non-patients on its use in Jordan, an area where data on this topic remain scarce.
Future studies could explore how the frequency and content of dermatological consultations influence long-term sunscreen use. Additionally, investigating whether similar trends exist in other sun-protective behaviors, like wearing protective clothing or seeking shade, would provide a more comprehensive view of photo protection practices.
CONCLUSION
This research studies different demographic, behavioral, and perceptual correlates of sunscreen use among dermatology patients in comparison with the non-dermatology population in Jordan. Sunscreen use was greater among women, those with lighter skin, higher education, and dermatologic patients, and better reapplication habits were observed. While the perception of the importance of sunscreen was high among participants, clear inadequacies in consistent sunscreen use, reapplication, and body site coverage were observed.
The results of this study highlight the importance of reaching high-risk groups through public health initiatives to increase sunscreen use, particularly in men, older adults, and people with darker skin. More efforts are needed to educate patients on the techniques of sunscreen application, reapplication, and the use of sufficient amounts of product to promote better sun protection.
A history of dermatology clinic visits was related to better sunscreen practices, supporting clinician-based advice in encouraging sun protection practices. In general, the findings presented in this study offer valuable perspectives for the design of more effective interventions to encourage regular and proper use of sunscreen, leading to enhanced skin health outcomes for disparate populations.
This study emphasizes the need for targeted education programs, especially for men, older adults, and individuals with darker skin tones, integrating sun safety measures into the community and implementing school-based programs to increase awareness of proper sunscreen habits from a young age. Public campaigns should address the misconception of low skin cancer risk. In addition, clinicians in all medical fields should be encouraged to provide counseling on sunscreen use during routine visits, and policymakers should consider making sunscreen more accessible through primary healthcare centers and lowering its price, especially in high UV seasons.
More research is needed to investigate other cultural, occupational, and behavioral contributors to the use of sunscreen and to test these associations in larger and more heterogeneous samples.
AUTHORS' CONTRIBUTIONS
The authors confirm their contribution to the paper as follows: R.A.N., A.M.A., N.A.: Study conception and design; L.M.J., Z.A.A.F.: Data collection; C.Y.S.: Analysis and interpretation of results; C.N.A.H.: Writing - Original Draft Preparation; S.M.Z.: Methodology. All authors reviewed the results and approved the final version of the manuscript.
LIST OF ABBREVIATIONS
| UVR | = Ultraviolet radiation |
| NMSC | = Non-melanoma skin cancer |
| WHO | = World Health Organization |
| JUH | = University of Jordan Hospital |
| IRB | = Institutional Review Board |
| SPF | = Sun protection factor |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
This study involved human participants and was reviewed and approved by the Institutional Review Board (IRB) of the University of Jordan Hospital, Jordan with Approval Number: [443/2025/67].
HUMAN AND ANIMAL RIGHTS
No animals were used in this research. All procedures performed in studies involving human participants were in accordance with the ethical standards of institutional and/or research committee and with the 1975 Declaration of Helsinki, as revised in 2013.
CONSENT FOR PUBLICATION
Informed consent was obtained from all participants. Confidentiality was maintained throughout the study.
AVAILABILITY OF DATA AND MATERIALS
The data supporting the findings of this article are available from the corresponding author, Dr. Ruby Abu Nassar, upon reasonable request.
ACKNOWLEDGEMENTS
Declared none.


